by Dr. Talia Marcheggiani, ND | Apr 21, 2015 | Botanical Medicine, cancer, Detoxification, Diet, Endocrinology, Fertility, Food, Health, Mental Health, Nutrition, Skin health, Weight Loss, Women's health
 Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.
Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.
Excess estrogen, especially in the form of these so-called “bad” estrogens, seems to be a common theme among women in North America. Stress, caffeine intake, synthetic estrogens in birth control pills and hormone replacement therapy and xeno-estrogens from cleaning products, plastics and cosmetics are among some of the causes of excess levels of estrogen in the body. Because of these environmental factors, many women suffer from something called “Estrogen Dominance”.
Symptoms of estrogen dominance include stubborn weight gain, anxiety, premenstrual symptoms of breast tenderness, acne, irritability, fatigue and brain fog. Estrogen dominance can contribute to worsening of health conditions such as infertility, fibrocystic breasts, repeated miscarriages, uterine fibroids and endometriosis as well as increase the risk of developing certain cancers.
Estrogen detoxification can be done effectively through a healthy diet that aims at improving estrogen clearance in the liver and regulation of the action of estrogen at cell receptors. By following this diet, patients can experience an improvement in hormonal health conditions, clearer skin and weight loss.
This diet is adapted from Dr. Joseph Collins RN, ND at yourhormones.com.
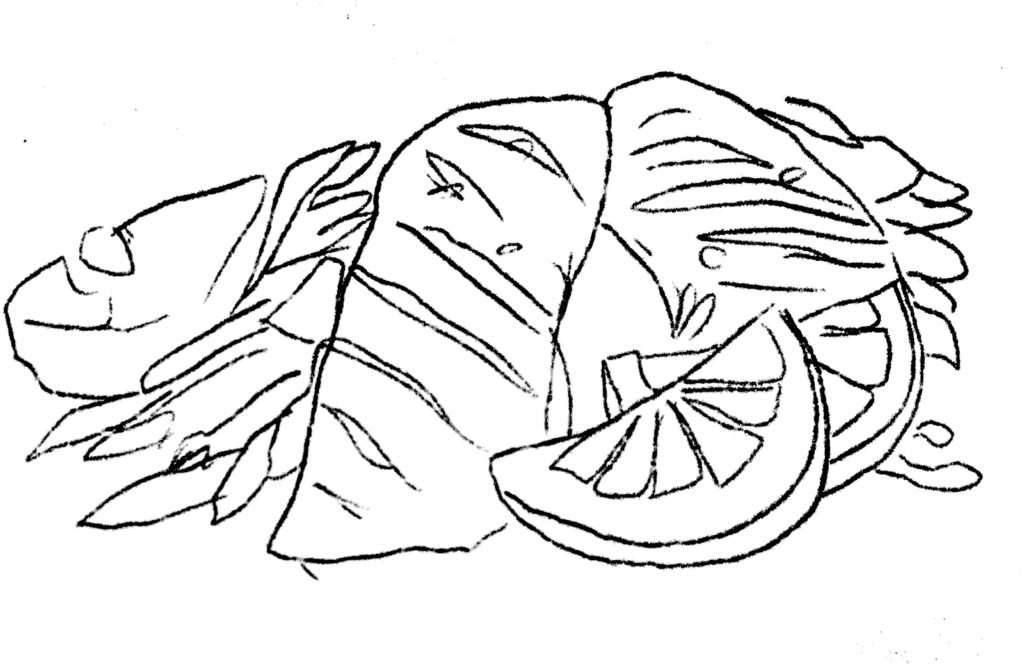
Cruciferous vegetables: Vegetables from the cabbage family, such as cabbage itself, cauliflower, broccoli, brussel sprouts, kale, bok choy, spinach, collard greens and other leafy greens are rich in a nutrient called indole-3-carbinol, or I3C. I3C gets converted to diindolymethane (DIM) in the body, which is responsible for clearance of excess estrogens in the liver. Consume a minimum of 3-4 servings of these vegetables per week.
Rosemary: Rosemary, when added to meats as a seasoning enhances the formation of good estrogens (the ones less likely to cause cancer or health concerns). Rosemary has the added benefit of antioxidant activity. It also enhances memory and mood and helps with thyroid function, improving weight loss, metabolism and energy levels.
Flaxseed: 2-4 tablespoons per day of ground flaxseed promotes healthy estrogen metabolism. The seed contains lignans, which help clear excess estrogens from the body. Flax also contains phytoestrogens, which control how much estrogen can bind to estrogen receptors. This means it can decrease excess estrogen activity or increase deficient estrogen activity, making it an effective remedy for a variety of female health complaints. Flax is rich in healthy omega-3 fats and contains fibre, making it an important remedy for treating inflammation and constipation. Flaxseed is digested and absorbed when ground, and best stored in the fridge as the oils in the seed quickly go rancid at room temperature.
Salmon and other fatty fish: Salmon and other fatty fish contain EPA, an omega-3 fatty acid, is an important anti-inflammatory oil. It has been shown to be effective in treating inflammatory conditions, cardiovascular disease and mental health conditions, such as depression, anxiety and ADHD. It helps increase the formation of “good” estrogens in the body. Enjoy 2-3 servings of fatty fish per week, or supplement with a quality fish oil.
Isoflavones: Isoflavones, such as those found in soy, are antioxidants effective at increasing good estrogens in the body. Since soy is often heavily processed, using herbs such as Trifolium pratense, Pueraria montana and Pueraria lobata either in teas, capsules or tinctures, will help provide an adequate dose of isoflavones.
Activated folic acid: Folic acid is responsible for converting estrogen into a very healthy, methylated form that can decrease the risk of certain cancers. Many people are unable to convert folate into the active 5-methyltetrahydrofolate, which is essential for hormone metabolism, DNA synthesis, homocysteine metabolism and nervous system function (good mental health, memory and energy). Other B vitamins to supplement with are B6 and B12 as they help folic acid metabolism estrogen into their anti-cancer form. Folic acid is found in dark leafy greens, which also contain your daily doses of indole-3-carbinol.
If you are experiencing symptoms of estrogen dominance in the form of a female health complaint, book an appointment to learn what else you can do to experience healthy, happy, pain-free periods and look and feel your best. Contact me.
by Dr. Talia Marcheggiani, ND | Mar 19, 2015 | Creativity, Diet, Endocrinology, Exercise, Fertility, Health, Lifestyle, Medicine, Mind Body Medicine, Nutrition, Paleo, Sex, Sexual Health, Skin health, Weight Loss, Women's health
 PCOS, or Polycystic Ovarian Syndrome, a condition which affects an estimated 10% of women in North America and is the most common endocrinological dysfunction in women.
PCOS, or Polycystic Ovarian Syndrome, a condition which affects an estimated 10% of women in North America and is the most common endocrinological dysfunction in women.
Its symptoms and the people it affects are as diverse as there are people affected; it’s one of my favourite conditions to treat.
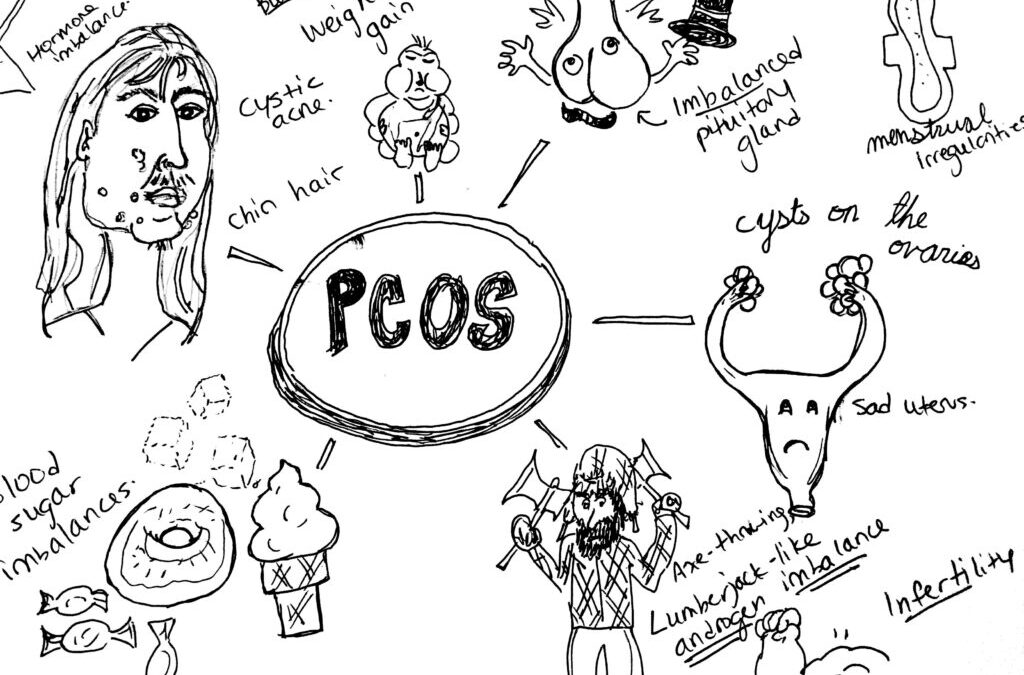
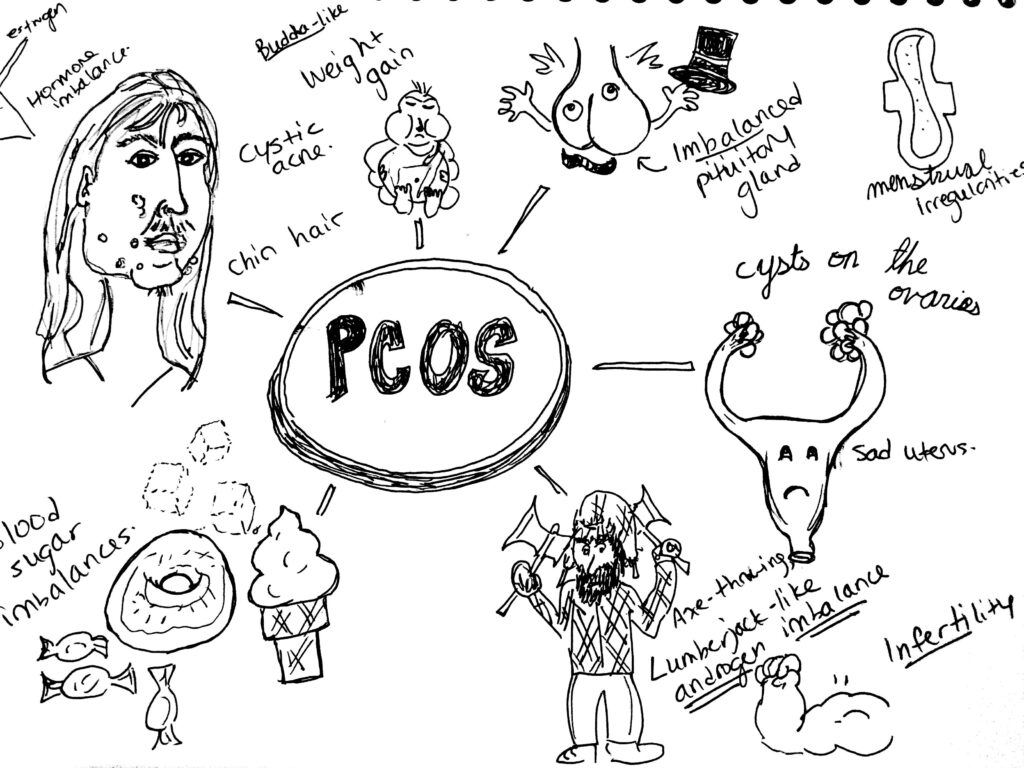
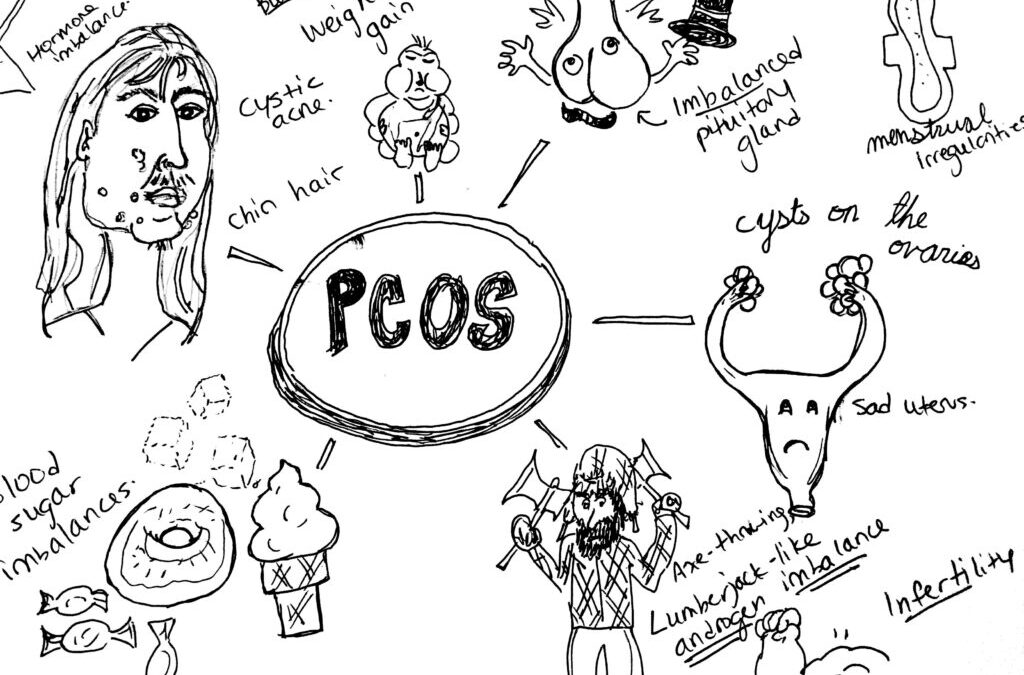
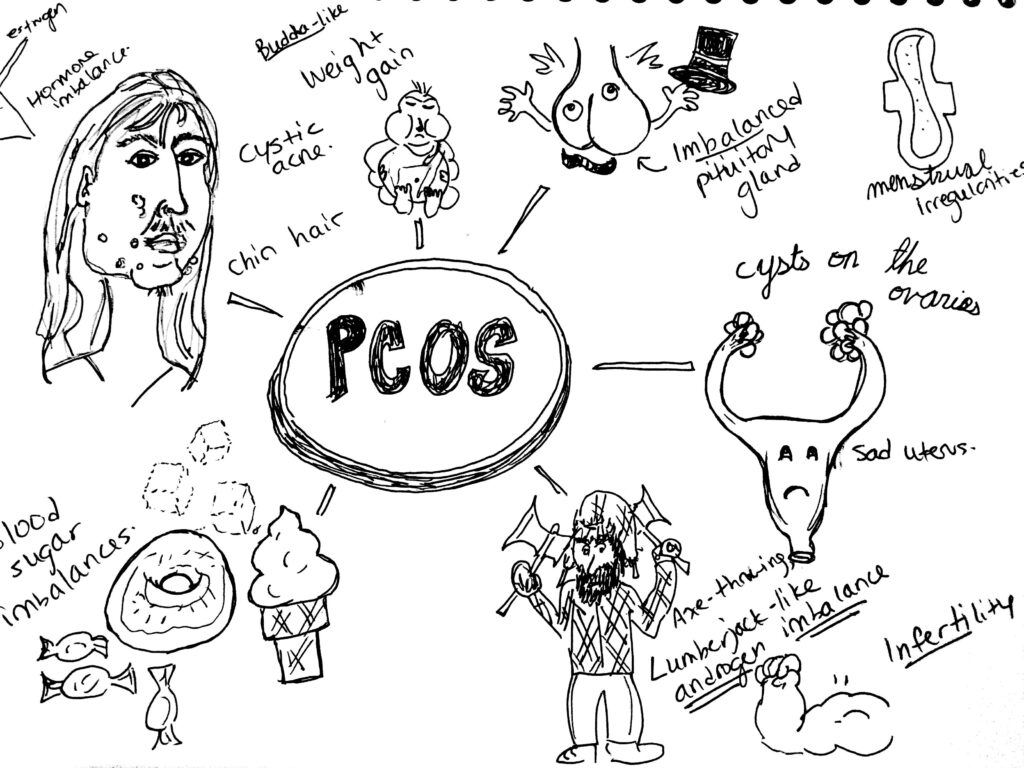
Signs and Symptoms:
PCOS is characterized by hormone dis-regulation. Oftentimes it presents with cysts on the ovaries, but not always. In PCOS there is often elevated blood glucose and other markers of insulin resistance. There are often issues with menstruation: the absence of periods (amenorrhea), or heavy and irregular bleeding (dysmenorrhea). Weight gain is common—although some women with PCOS can be thin—as is hormonal acne and hirsutism, a nice word for male-pattern hair growth: excess hair growth around the chin and upper lip, the chest or navel region. Pelvic pain around ovulation may occur when cysts rupture. Infertility is common in women with this condition.
PCOS is a syndrome, rather than a disease, which means it presents as a collection of symptoms that can be varied in their presentation and severity. Lab work may read that estrogen, testosterone and LH (a hormone produced by the pituitary gland and ovaries) are high and progesterone and FSH (a hormone released by the pituitary gland) are relatively low. However, what brings a woman with PCOS or PCOS-like symptoms into my office is varied and usually consists of any combination of visible symptoms: hair growth, weight gain, acne, menstrual irregularities or infertility.
Etiology:
We are uncertain how the collection of symptoms that is PCOS arises. One prominent theory is that issues with blood sugar and insulin regulation create ovarian cysts or disruptions in the secretion of sex hormones. This causes the ovaries to release more LH, which has the power to raise testosterone. High insulin, testosterone and estrogen can cause weight gain, hair-growth, acne, absence of ovulation (anovulation) and the inability to maintain the uterine lining and therefore carry a pregnancy to term.
Diagnosis:
PCOS is diagnosed by symptoms. It involves a combination of symptoms: amenorrhea (or absence of menstrual periods), infertility, hair growth on the face, acne and insulin resistance. The presence of ovarian cysts, as detected on an ultrasound were once diagnostic, but many patients present with symptoms and are cyst-free. An increase in LH and testosterone, with lab values indicating insulin resistance and metabolic syndrome, can also lead doctors to suspect PCOS, when appearing in conjunction with other symptoms.
Because it is a syndrome, patients often come into my practice with a variety of complaints. Some come in to deal with their skin health, others want help with fertility or menstrual cycle regulation and many others come in with weight loss goals.
Conventional Treatment:
Treatment in conventional medicine is simple: oral contraceptives. If your testosterone is high and estrogen and progesterone are out of whack, the conventional medical system tells us to simply override natural hormone production, or lack thereof, with synthetic versions of the same thing. For my professional opinion on regulating hormones with oral contraception, see my post on the birth control pill (which I no longer take). These birth control pills often contain chemicals that prevent the secretion of male hormones. This helps clear up acne and hair growth.
Medication for type II diabetes, Metformin, is used to help regulate insulin. Patients experience weight loss on Metformin, as it helps control insulin resistance, however it also depletes vitamin B12, which means that regular injections of B12 are necessary to avoid deficiency symptoms. Further, Metformin doesn’t address the root cause of insulin resistance, which is most likely lifestyle and hormonal imbalance. This means that patients will be medicated (and therefore receiving B12 injections) for life.
I do not mean to negate the fact that oral contraception and Metformin have helped countless women. I respectfully acknowledge the fact that the lens I look through is one of a different, more natural and whole-bodied approach to medicine that aims to treat the individual by addressing the root cause of disease.
In short: I prefer to try it the naturopathic way first.
Naturopathic Treatment:
Lifestyle. Naturopathic remedies are very effective, but often quite involved. They begin with lifestyle modifications—a low glycemic index diet like the Mediterranean or the Paleo diets, that emphasize whole foods, like fruits, vegetables, healthy fats and lean protein and eliminate sugar, white flours and white carbohydrates. Exercise is important in treating PCOS. One of my professors advocates intense cardio, such as high-intensity interval training, or weight-lifting 5-6 days a week. This must be done for several months before effects are seen and blood sugar and other hormones are regulated.
Supplementation and botanicals. Myo-inositol, a B vitamin, is a first-line treatment for PCOS in the natural health world. The amount of research steadily growing behind its use should probably make this gentle and effective treatment first-line for treating PCOS in all healthcare fields. Studies show that, when dosed properly, inositol can regulate blood sugar, assist with weight loss and regulate menses, even promote fertility.
Herbs like Vitex agnus-castus, or chaste tree, can help regulate the balance between estrogen and progesterone. Spearmint and Serenoa repens, or saw palmetto, can help decrease male hormones in the body. Gymnema and berberine are other therapies useful for regulating blood sugar and helping with weight loss.
Ensure that you are receiving counsel from a licensed naturopathic doctor before supplementing. The dose and quality of supplements and herbs is essential to feeling better—don’t hack it in the health food store alone!
Acupuncture. Acupuncture has been shown to be effective for promoting fertility. I have had some good success in promoting pregnancy and fertility with acupuncture in my practice. Fertility clinics in Canada now use acupuncture before and after IVF treatments to ensure treatment success. It also helps to relieve stress and lower cortisol, which helps with insulin-lowering and blood sugar management.
In Traditional Chinese Medicine, PCOS can manifest as dampness, Qi or yang deficiency or issues with the Spleen or Kidneys. Acupuncture can help tonify and balance these patterns.
Homeopathy. I have had success using homeopathy in conjunction with lifestyle and supplementation in treating PCOS. Homeopathy acts deeply on the energetic level of disease, working on the level of emotions and sensations and working to address the energetic cause of disease. It involves a thorough interview and an individualized prescription from a licensed naturopathic doctor or homeopath.
Mind-Body Medicine. The ovaries are located at the level of the second chakra, which is an energetic centre in the body associated with sexuality and creativity. Christine Northrup, MD, asserts that the presence of ovarian cysts represents an energetic blockage in our creative power and unmet emotional needs. Louise Hay, author of “You Can Heal Your Life” tells us that ovarian cysts represent some sort of past hurt that we can’t let go of. Crying, journalling and identifying repressed emotions can help to remove these energetic blockages. In many women with PCOS, there is an imbalance in the identification with their femininity, or what it means to be a woman.
Sometimes our bodies alert us of imbalances in our emotional lives through the presence of physical symptoms. As a naturopathic doctor, it is essential I address all levels of the person—mentally, emotionally and spiritually, not simply physically.
PCOS is a diverse and challenging condition to treat that can cause a lot of hardship for the women who suffer from it. However, a diagnosis of PCOS can be an opportunity for growth and transformative healing through naturopathic medicine. For this reason, I find it can be one of the most interesting and rewarding conditions to treat. Contact me to find out more.

by Dr. Talia Marcheggiani, ND | Nov 7, 2014 | Endocrinology, Fertility, Hormones, Sexual Health, Sexuality, Weight Loss, Women's health
 There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
I’m surprised to find that I’m hesitant to admit it publicly, but I’ve decided to go back on The Pill after considering various contraception methods; in natural health circles the Birth Control Pill is often seen as an unnecessary evil. However, Tori Hudson author of the Women’s Encyclopedia of Natural Medicine, has called oral contraceptives a “truly revolutionary option for women” and points out that the dose of estrogen and progesterone in the pill today is much lower than it was when it first arrived on the market. That being said, it’s important to talk to a healthcare provider to go over birth control methods and decide which one is right for you. Alternate options include physical barriers, such as condoms and diaphragms, cycle charting, apps, such as the Lady Comp, or IUDs, to name a few. Each method has its associated pros, cons, costs and health risks. Finding a safe and effective form of contraception involves you and your healthcare team.
For me, The Pill seems to be the best choice at the moment for various reasons, which I won’t get into here. However, the idea of ingesting synthetic hormones again, after having carefully brought my cycles back to a perfect, painless and PMS-free 28-day rotation and after having cleared up my hormonal acne, made me nervous. So, I did what all trained naturopathic doctors do; I used my naturopathic know-how to tailor an optimal Synthetic Hormonal Experience for myself. Going back on the pill needn’t come with undesirable side effects; maybe it could be a positive experience. Here are some tips:
Decide if oral contraception is your best method
Selecting the method of birth control that best fits your lifestyle, budget, health history and personal style requires an in-depth conversation between you and your healthcare provider. He or she should have a detailed conversation with you about your expectations, goals, sexual and health history as well as family history. Selecting the right method may also require some trial and error.
Consider the associated risks
A history of smoking and blood clots could put you at risk for dangerous side effects. The birth control pill is also associated with an increased risk of certain cancers. (And a decreased risk of uterine and ovarian cancers in the general, healthy population). Your personal risk profile will involve your personal health history and family history as well as lifestyle factors such as smoking. Talk to your healthcare provider.
Pick the right pill for you
Based on my history of suboptimal glucose control, hormonal acne and irregular periods, I knew that I needed a pill with the lowest dose of estrogen possible. My hormonal profile tends towards estrogen dominant and progesterone deficient so I chose a low-dose estrogen and high-dose progestin pill. The form of progestin used has zero androgen (male hormone) activity, therefore it is unlikely to contribute to acne. It also contains a diuretic, which combats my tendency to hormone-related water-retention. The combination of my knowledge of my personal hormonal profile and ability to research hormone combinations in various pills led me to choose a product that offered positive side-effects rather than negative ones. Since being on the pill again, I’ve experienced weight loss, rather than gain, lighter, more regular cycles and clearer skin. It’s worth repeating that these side-effects were not my motivation for going on the pill. If you are using the pill for symptom-management and hormone-balancing rather than birth control, consider trying natural methods instead.
Be prepared for trial and error-ing as hormone levels fluctuate
Give your new pill a 3-month trial period. During this period, be prepared for temporary side effects such as mood changes, skin outbreaks, temporary weight gain or water retention and break-through bleeding. Other common side effects of synthetic hormones are nausea and headaches. Allow 3 months for things to stabilize and, if still experiencing symptoms, talk to your healthcare provider about trying a new pill or birth control method.
Make sure to supplement to account for vitamin and mineral deficiencies
Oral contraceptives can deplete several key vitamins and minerals. The B vitamins folate, B6 and vitamin B12 are most notably affected. Deficiencies in these vitamins could lead to fatigue and depression or even neurological impairment. Magnesium, zinc and vitamin C levels are also affected, which can have an impact on the immune system. These minerals are important in a variety of metabolic processes. Since starting the pill again, I am diligent about taking my B-complex and magnesium supplements. Make sure you talk to your naturopathic doctor or other healthcare provider about choosing a quality supplement and dosing correctly, to make sure you are putting back in your body the nutrients that your pill may be depleting.
Hormone balance when coming off the pill
If you reach a happy medium with your pill, then congratulations! But, you ask, what happens if I decide to get pregnant or switch to another method of birth control? Work with a naturopathic doctor or your trusted healthcare provider to balance hormones with herbal or nutritional supplements when coming off of the pill. Herbs such as vitex, help regulate hormones and prevent side effects from the withdrawal of synthetic hormones.
For more information on balancing hormones and optimizing fertility, contact me.
This article is not a substitute for medical advice.
 Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.
Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.