by Dr. Talia Marcheggiani, ND | Nov 16, 2015 | doctor as teacher, Education, Emotions, Endocrinology, Healing Stories, Hormones, Listening, Medicine, Meditation, Mind Body Medicine, Naturopathic Philosophy, Preventive Medicine, Reflections, Women's health, Writing
Premature Ovarian Failure no longer bears that name. It’s not a failure anymore, but an insufficiency. POF becomes POI: Premature Ovarian Insufficiency, as insufficiency is apparently a softer term than “failure”. For me, it’s another telling example of how our society fears the names of things, and twists itself into knots of nomenclature and terminology rather than facing pain head-on. In this case, the pain is derived from the simple fact that the ovaries do not respond to hormones, that they for some reason die at an early age and cause menopause to arrive decades before it’s due, leading to infertility and risk of early osteoporosis.
Insufficiency, for me at least, fails to appease the sensitivity required for naming a problem. It reminds me of a three-tiered scoring system: exceeds expectations, meets expectations, insufficient performance. These reproductive cells have not been up to task. They’ve proven to be insufficient and, in the end, we’ve labelled them failures anyway—premature ovarian disappointments. Our disdain for the bodies we inhabit often becomes apparent in medical jargon.
What expectations do we have for our organs, really? For most of us that they’ll keep quiet while we drink, stay up late and eat what we like, not that they will protest, stop our periods, make us itch or remind us that we are physical beings that belong here, to this earth, that we can sputter and shut down and end up curb side while we wait for white coats to assist us. Our organs are not supposed to remind us of our fragile mortality. When it comes to expectations overall, I wonder how many of them we have a right to.
In one week I had two patients presenting with failures of sorts. With one it was her ovaries, in another it was his kidneys, first his left, now his right. Both of them were coming to me, perhaps years too late, for a style of medicine whose power lies mainly in prevention or in stopping the ball rolling down the hill before it gains momentum. When disease processes have reached their endpoint, when there is talk of transplant lists and freezing eggs, I wonder what more herbs can do.
And so, when organs fail, I fear that I will too.
In times of failure, we often lose hope. However, my patients who have booked appointments embody a hope I do not feel myself, a hope I slightly resent. In hope there is vulnerability, there is an implicit cry for help, a trust. These patients are paying me to “give them a second opinion”, they say, or a “second truth”.
I feel frustration bubble to the surface when I pore over the information I need to manage their cases. At the medical system: “why couldn’t they give these patients a straight answer? Why don’t we have more information to help them?” At my training: “Why did we never learn how to treat ovarian insufficiency?” At the patients themselves: “Why didn’t he come see me earlier, when his diabetes was first diagnosed?” And again at the system: “Why do doctors leave out so much of the story when it comes to prevention, to patient power, to the autonomy we all have over our bodies and their health?” And to society at large: “Why is naturopathic medicine a last resort? Why is it expensive? Why are we seen as a last hope, when all but the patients’ hope remains?”
Insufficiency, of course, means things aren’t enough.
I feel powerless.
There is information out there. I put together a convincing plan for my patient with kidney failure. It will take a lot of work on his part. What will get us there is a commitment to health. It may not save his kidneys but he’ll be all the better for it. My hope starts to grow as I empower myself with information, studies some benevolent scientists have done on vitamin D and medicinal mushrooms. Bless them and their foresight.
As my hope grows, his must have faded, because he fails to show for the appointment. I feel angry, sad and slightly abandoned—we were supposed to heal together. Feelings of failure are sticky, of course, and I wonder what story took hold of him. was it one that ended with, “this is too hard?” or “there is no use?” or “listen to the doctors whose white coats convey a certainty that looks good on them?”
A friend once told me, the earlier someone rejects you, the less it says about you. I know he’s never met me and it’s not personal, but I take it personally anyways, just as I took it personally to research his case, working with a healing relationship that, for me, had been established since I entered his name in my calendar. In some way, like his kidneys, I’ve failed him. Since we’re all body parts anyways, how does one begin to trust another if his own organs start to shut down inside of him? Why would the organs in my body serve him any better than the failing ones in his?
I get honest with my patient whose ovaries are deemed insufficient (insufficient for what? We don’t exactly know). I tell her there aren’t a lot of clear solutions, that most of us don’t know what to do–in the conventional world, the answer lies mainly in estrogen replacement and preserving bone health. I tell her I don’t know what will happen, but I trust our medicine. I trust the herbs, the homeopathics, nutrition and the body’s healing processes. I admit my insufficiency as a doctor is no less than that of her ovaries, but I am willing to give her my knowledge if she is willing to head down this path to healing with me. Who knows what we’ll find, I tell her, it might be nothing. It might be something else.
It takes a brave patient to accept an invitation like the one above; she was offered a red pill or a blue pill and took a teaspoon of herbal tincture instead. I commend her for that.
There aren’t guarantees in medicine but we all want the illusion that there are. We all want to participate in the game of white coats and stethoscopes and believe these people have a godlike power contained in books that allows them to hover instruments over our bodies and make things alright again. Physicians lean over exposed abdomens, percussing, hemming and hawing and give us labels we don’t understand. The power of their words is enough to condemn us to lives without children, or days spent hooked up to dialysis machines. We all play into this illusory game. They tell us pills are enough… until they aren’t. This is the biggest farce of all.
I can’t participate in this facade, but I don’t want to rob my patient of the opportunity for a miracle, either. We share a moment in the humility of my honesty and admission of uncertainty. I know my patients pay me to say, “I can fix it.” I can try, but to assert that without any degree of humility would be a lie. How can one possibly heal in the presence of inauthenticity? How can one attempt to work with bodies if they don’t respect the uncertain, the unknown and the mysterious truths they contain? In healing there is always a tension between grasping hope and giving in to trust and honestly confessing the vulnerability of, “I don’t know.”
For my patient I also request some testing—one thing about spending time on patients’ cases and being medically trained is that you get access to information and the language to understand it. I notice holes in the process that slapped her with this life-changing diagnosis.
When her labs come back, we find she might not have ovarian insufficiency after all. Doorways to hope open up and lead us to rooms full of questions. There are pieces of the story that don’t yet fit the lab results. I give her a list of more tests to get and she thanks me. I haven’t fixed her yet, but I’ve given her hope soil in which to flower. I’ve sent her on a path to more investigations, to more answers. And, thanks to more information in the tests, I’ve freed her and her ovaries from the label of “failure” and “insufficient” and realized that, as a doctor, I can free myself of those labels too. The trick is in admitting, as the lab results have done in their honest simplicity, what we don’t know.
For the moment, admitting insufficiency might prove to be sufficient in the end.

by Dr. Talia Marcheggiani, ND | Oct 9, 2015 | Acupuncture, Autoimmune, Detoxification, Diet, Digestion, Elimination Diet, Endocrinology, Fertility, Fitness, Food, Food Sensitivities, Gluten Free, Health, Hormones, Nutrition, Stress, Weight Loss, Women's health
 This is a common story that can describe any number of patients I see in my private practice: My patient has been doing well–she’s been exercising regularly; she’s been cutting out sugar and processed foods and watching what she eats. She’s been having salads for lunch. She’s even gotten her husband on board! He’s started to have salads for lunch with his cheeseburger (instead of fries) and given up having a row of cookies in the evening. All things considered, she’s been doing great. However, despite her best efforts, after one month of tiresome slog, restriction and dedication, she’s only managed to lose a few pounds. Her husband? He’s lost 10.
This is a common story that can describe any number of patients I see in my private practice: My patient has been doing well–she’s been exercising regularly; she’s been cutting out sugar and processed foods and watching what she eats. She’s been having salads for lunch. She’s even gotten her husband on board! He’s started to have salads for lunch with his cheeseburger (instead of fries) and given up having a row of cookies in the evening. All things considered, she’s been doing great. However, despite her best efforts, after one month of tiresome slog, restriction and dedication, she’s only managed to lose a few pounds. Her husband? He’s lost 10.
“He has more to lose,” I suggest to her. “Those few pounds you’ve lost are gone for life—slow and steady stays off forever.” I am her cheerleader, but the truth is: hormones, especially when it comes to women.
Hormones are the body’s telegrams. They are produced in glands in tissue like the gut, ovaries, adrenals and brain and act on distant cells in the body, telling them how to behave. When it comes to weight loss, hormones can be the culprit if diet and exercise have failed to produce results. Hormones control appetite, mood, food cravings, metabolic rate, fat gain and distribution and hunger, among other things. Any hormonal imbalance will sabotage weight loss efforts and it’s often the first place I look when a patient has weight loss goals that they aren’t achieving with diet and exercise alone.
The Players:
There are numerous hormones in the body that are responsible for the above actions, however the main ones that we can affect through diet and lifestyle are insulin, cortisol, estrogen and the thyroid hormones. These are just some key players in a team, however just by working on these four, we can start to see results.
Interconnectedness:
Hormones are complex entities, not only for the wide array of effects, but for their tendency to effect the action of each other. For example, high cortisol can effect levels of estrogen, insulin and the thyroid hormones. High insulin can affect cortisol and estrogen. And so on. Working on hormones is like attacking a giant knot and often requires starting from the basics: diet and lifestyle.
Insulin Imbalance:
Insulin is an important hormone in the body—we can’t live without it. Released by the pancreas after a carbohydrate-rich meal in response to rising levels of sugar in the blood, insulin gets sugar into cells where it can be used as fuel. It also brings down blood sugar, making it a main culprit in hypoglycemic crashes and sugar cravings. The problem with insulin, however, is when we overeat carbohydrates and sugar, we overuse the insulin response. The result is abdominal fat, weight gain (insulin tells the body to store fat), a blood sugar roller coaster, mood swings (that “hangry” feeling) and intense sugar cravings and energy crashes.
Balancing Insulin:
Insulin is best balanced by diet, particularly managing carbohydrate intake and emphasizing healthy fats and protein in the diet. Fat and protein slow sugar absorption. This prevents a rise in blood sugar and decreases the need for insulin. The result is feeling satiated for longer, having stable energy and decreasing food cravings.
Morning protein:
The first step in balancing insulin release is to increase morning protein. I recommend aiming for 30 g of good quality, lean protein for breakfast like a chicken breast, or scoop of whey isolate protein powder in a whole foods smoothie. I was once accused jokingly of “not knowing that breakfast is”, when recommending chicken breasts for breakfast. However, perhaps it’s North America that has a skewed sense of what makes a decent morning meal. If the aim of breakfast is to break the fast that you’ve had throughout the night, then starting it off with a high-carb, high-sugar, nutrient-sparse piece of toast or bowl of breakfast cereal seems crazy to me. In Colombia and India, two places I’ve spent some time, we started off the day with a protein-rich stew or meat soup.
To balance insulin make sure that every meal, even snacks, contain some form of protein or a fat. Avoid eating carbohydrates by themselves and keep servings of carbs to a minimum and in their unprocessed, whole form (like large flake oats, quinoa and brown rice as opposed to flours or cereals).
Cortisol Imbalance:
One of the main hormone imbalances I notice when it comes to stubborn weight gain is cortisol imbalance. Cortisol is the stress hormone. It’s released by the adrenal glands, two pyramid-shaped endocrine glands that sit on top of the kidneys, in response to stress. Animals have two modes of operation: fight or flight or rest and digest. Cortisol increases blood sugar and alertness and tells the body to divert attention to gearing us up for combat or escape, and moves us away from investing energy in digestion, immunity and concentration. Cortisol is a wonderful hormone; it keeps us awake, and makes us feel alert and well, priming us to be effective in our busy, stressful lives. However, our bodies weren’t made for long-term stress response and we spend most of our time in fight or flight mode.
Cortisol and blood sugar:
Cortisol raises blood sugar, causing insulin to be released. This starts us on a blood sugar roller coaster trip, leading to sugar cravings, energy crashes and storing fat.
Cortisol and fat distribution:
Cortisol doesn’t directly tell the body to store fat (it happens through other mechanisms that happen in response to high cortisol), but it does encourage fat redistribution. Cortisol tells the body to move fat from the hips and thighs and deposit in the abdomen, face and shoulders, leading to the sexy “Buffalo Hump”. We know that abdominal fat carries more health risks than fat in other areas of the body so this detail can be troublesome when it comes to long-term effects.
Cortisol and the thyroid:
Cortisol impacts the thyroid by preventing the conversion of T4 to the more active T3. T3 and T4 are important thyroid hormones that set the body’s metabolic rate, among other things.
Cortisol and the sex hormones:
Cortisol can lead to estrogen dominance by diverting resources away from estrogen and progesterone production. In menopause, this is particularly troublesome, as the body relies on the adrenal glands, rather than the ovaries, to produce the sex hormones. High cortisol can result in progesterone deficiency and estrogen dominance symptoms, which can negatively affect weight loss. Cortisol also causing accelerated aging and who wants that?
Cortisol Balancing:
The main thing when it comes to cortisol balancing is to Calm Down—or as I like to poignantly put it, Calm the F#$% Down. The way this is done is highly individualized. Some recommendations I have are: meditation, yoga, exploring acupuncture (a wonderful way to balance cortisol, among other things), journaling, taking a day off, re-evaluating priorities at work and at home, etc. Mainly, getting 7-9 hours of sleep a night is essential for managing the stress response.
Taking it easy:
When it comes to weight loss, I often notice that certain efforts hinder our progress. It’s important to keep caloric intake adequate—eating too few calories can stress the body out, causing cortisol release. It’s also important to manage exercise. While exercise can teach the body how to manage stress, it does produce cortisol in the short-term. Therefore it’s important to keep exercise short and intense. Weight-training, short bursts of cardio (no more than 20 minutes) and varying intensities with High Intensity Interval Training, Tabata or Crossfit, are the best choices for weight loss. Training for a marathon or long-distance bike race may be fun and fulfilling, but they are not the best choices for weight loss, as they prolong the stress response and can work against you, rather than in your favour.
When I have a patient who is intensely tracking what they eat and over-exercising my advice is often (and it’s not that well-received, as you can imagine) “Take it easy”. Easing up on exercise and relaxing calorie-counting may be hidden pieces in the weight loss game.
Herbs and supplements:
There are a variety of nutrients to take to support adrenal function. The main things to consider, with the advice and counsel of a trained naturopathic doctor are B-vitamins, magnesium and adaptogenic herbs (the help the body adapt to stress).
Estrogen Dominance:
Estrogen, actually a group of hormones, are female sex hormones. Their main job is to promote the expression of female sex characteristics, the growth of breast tissue and to control ovulation. Estrogen also causes body to fat to be distributed to the thighs, buttocks and lower abdomen. The problem with modern society is an imbalance in the two female sex hormones, estrogen and progesterone. Due to stress and toxic environmental estrogens, or xenoestrogens, among other things, modern women have more estrogen relative to progesterone in their bodies. The effects of this are numerous and include, stubborn weight gain in the thighs (the famed “saddlebags), cellulite, acne, PMS, painful menstrual periods, fibroids, hormonal conditions such as PCOS, and the occurrence of certain female cancers, especially breast cancer. Estrogen can also contribute significantly to anxiety symptoms.
Estrogen balancing:
Correcting estrogen dominance primarily involves supporting estrogen detox pathways in the liver. Chemicals such as I3C, DIIM and calcium-d-glucarate help increase the liver’s ability to clear foreign estrogens from the body. Supporting digestive health also allows us to remove estrogens—they are neutralized in the liver and eliminated through the colon. Leafy greens contain a high amount of these chemicals, so ensuring you get adequate amounts in your diet is important for estrogen metabolism. Ground flaxseed, rosemary and fish oil are also important nutrients for clearing excess estrogen from the body.
Reducing exposure:
Try to reduce exposure to foreign estrogens by avoiding the use of plastic bottles and plastic-lined cans, using natural skincare and body products and natural cleaning aids whenever possible. It’s also important to see a naturopathic doctor 2-4 times a year for a medically-assisted natural detoxification to clear the body of toxic estrogens.
Hypothyroidism:
The thyroid gland sits on the neck, just below the Adam’s Apple. It releases two hormones T4, and the more active T3. These hormones are responsible for setting the body’s metabolic rate—converting fat into heat and energy. Thyroid deficiency, or hypothyroidism is more common in our society than we think (naturopathic doctors have stricter criteria for laboratory reference ranges than conventional medicine—we look for signs of health, not disease). Conventional medicine deems hypothyroidism as having a TSH (thyroid stimulating hormone) level above 5—for this hormone, all you need to know is lower is better—however ND’s will start to treat the thyroid when symptoms are present and TSH is above 2.5. Symptoms of hypothyroidism are stubborn weight gain, constipation, feeling cold, fatigue, especially brain fog, weak memory, hair loss, dry skin and thinning of the eyebrows.
Supporting the thyroid:
The thyroid gland is a fragile organ, sensitive to inflammation and stress. When there is inflammation in the body, often caused by stress, diet or insulin resistance, the thyroid is the first gland to suffer. Most cases of hypothyroidism are autoimmune in nature. Therefore, naturopathic doctors aim to correct inflammation by prescribing an anti-inflammatory diet and looking for food sensitivities. When we identify food sensitivities (through specialized IgG antibody testing or an elimination diet) and remove them from the diet, we can focus on gut healing which treats inflammation and helps repair the thyroid.
Managing stress:
Low calorie diets have the effect of suppressing thyroid function, which leads to the yo-yo dieting effect. Avoid extremely low calorie diets, or opt for intermittent fasting or calorie-cycling instead. Aim for slow and steady weight loss so as not to harm metabolic rate, which makes weight loss more difficult in the long run.
I previously mentioned that cortisol can harm the thyroid and that hormones are interlinked. Cortisol prevents the conversion of T4 to the more active T3, which can slow metabolism.
Nutrients:
A deficiency in iodine, zinc, iron and selenium, among other nutrients, can negatively impact the thyroid. Talk your naturopathic doctor about testing and supplementation.
Summary:
What would a visit to a naturopathic doctor look like? When it comes to hormones, treatment is often complex as it targets the root cause of symptoms and involves detangling the complicated web of hormones that are at play. This can require some diagnostic detective work. A naturopathic doctor will take your complete health history, order labs and perform physical exams if necessary. A common treatment plan might look like this:
- Sleep: 7-9 hours per night
- Take stress seriously: sign up for a round of acupuncture, start meditation, do yoga, journal, etc.
- Measure hormones via saliva: cortisol, testosterone, DHEA, estrogen, progesterone
- Identify food sensitivities via an elimination diet or an IgG Food Panel that tests for antibodies to certain foods in the blood.
- Correct nutritient deficiencies through diet and supplementation
- Herbs for hormonal support: estrogen detoxification, thyroid support, gut healing, adrenal support, glucose control and blood sugar balancing.
- Exercise: short, intense bursts that target muscle-building
- Diet: high protein, especially in the morning, healthy fats, low carbs and eliminate sugar, processed foods and food sensitivities.
To learn more about how naturopathic medicine can help you lose weight, balance hormones and fight disease, contact my clinic Bloor West Wellness at 416 588 0400 to set up an initial appointment. Let’s get started today!
Want to balance your hormones, energy and mood naturally? Check out my 6-week foundational membership program Good Mood Foundations. taliand.com/good-mood-learn

by Dr. Talia Marcheggiani, ND | Aug 25, 2015 | Botanical Medicine, Cold and Flu Remedies, Detoxification, Digestion, DIY, Fertility, Herbalism, Hormones, Medicine, Mental Health, Mind Body Medicine, Recipes, Skin health, Women's health

As a student of naturopathic medicine, I didn’t quite get herbs. They were natural, sure, but why would I prescribe them in lieu of homeopathy, dietary changes or nutritional supplements? I didn’t get it.
I liked herbs; I understood the idea of synergy—the fact that the effect of the entire plant is greater than the sum of its parts. Also, I knew that plants often have superior effects to some drugs in that they often contain active ingredients that balance the side effects otherwise caused by most pharmaceutical medications. For example, anti-inflammatory herbs like turmeric and licorice root also support and strengthen the immune system, rather than suppress it, as most anti-inflammatory drugs tend to do. For most drugs that lower inflammation, a common side effect is severe immune deficiency. This is not the case for herbs that lower inflammation, which actually benefit the immune system. So, I knew herbs were cool.
I also liked the idea that each tincture was individually created for the totality of symptoms a patient presented with. Creating a specific medicine for each individual seemed to fit with the idea of singularity in medicine, which I resonated with. However, for a long time I didn’t get herbs. And I’ve often been reluctant to prescribe herbs in my practice.
First of all, I don’t have my own dispensary so sending patients off to buy tinctures created a kind of disconnection from the source of my prescriptions. Secondly, as many of you who have tried it can contest, tinctures (or herbs extracted in alcohol) taste terrible and make compliance hard, even for myself. Thirdly, tinctures are quite expensive. Each 50 ml of tincture can cost upwards of $5 making a month’s supply of herbs quite costly. This is funny because many of the herbs that are so costly to buy grow like weeds in southern Ontario (dandelion, for example, is often considered a weed) and tinctures aren’t that difficult to make. Fourthly, I didn’t like to prescribe tinctures because, as I understood it, people would only feel better while actively taking the herb. In my mind, the herb worked like a drug in that once you stopped taking it, the positive effects would diminish. This differed from my understanding of homeopathy, which stimulates the body to heal itself, correcting nutritional deficiencies or looking for and treating the root cause of symptoms. I doubted whether the way we were taught to prescribe herbs did in fact treat the root cause. This is important because the guiding principles of naturopathic medicine dictate that we aim to do this whenever possible.

I had no doubt, however, that herbs were effective. Taking a tincture seemed to be far more effective for me and the patients I treat than taking supplements. Herbs are nutritional—they are a food and a medicine and therefore contain a myriad of health benefits beyond treating what they are prescribed to treat.
It wasn’t until I read author and herbalist Matthew Wood’s works on herbalism that I began to internalize the idea that herbs do in fact stimulate the body to heal itself. Plants contain an inherent wisdom, according to Wood and his studies in western and Native American herbalism. Plants eradicate disease by stimulating the healing powers of the body and strengthening the body’s capacity to heal itself from disease. The body is constantly trying to heal itself from ailments and, when these processes become blocked for one reason or another, disease symptoms begin to manifest. Herbs can strengthen the body’s healing processes, when prescribed in a certain way, and large doses for long courses of time are not necessary. Further, once the disease is eradicated, the herbs can be stopped. When prescribed as a healing catalyst, disease doesn’t return once the herbal prescriptions have done their work.
Wood writes, “It should be understood that herbs can be used either way: to stimulate the self-healing powers of the organism to return to health, or to artificially manipulate the organism to fit an artificial goal.” He uses the examples of goldenseal, which at high doses can kill bacteria or viruses that have invaded the body and in smaller doses can increase the mucosa and digestive systems of the body to rid itself of the invaders and, in turn, strengthen the body against future invasions.
In regards to the cost of herbal tinctures, there are relatively simple ways to get the effects of herbs by making your own tinctures.
Read on to support liver detox, hormonal health and cardiovascular health by creating your own rosemary tincture using dried rosemary, one of my favourite herbs of the moment, and a bottle of white wine:
Rosmarinus officinalis, is the latin name for rosemary, a member of the mint family. While better known for its ability to perfectly complement roast chicken, it has a number of health benefits. Rosemary’s energetic actions are stimulating and warming, according to Matthew Wood. It clears up phlegm and dampness, stagnation and sluggishness in the tissues.
Rosemary has the ability to boost metabolism and increase the absorption of sugars and fats, which make it an appropriate nutritional supplement for people with diabetes. It can help drive glucose into the cells, diminishing the need for the body to release large amounts of insulin, re-sensitizing cells to insulin and lowering blood sugar. It can help nourish the entire body and has a special affinity for the heart, lungs, spleen, liver and kidneys.
Rosemary is currently often used to detoxify toxic, exogenous estrogens from the body while promoting the conversion of health-promoting estrogens in the liver. It is a powerful stimulator of liver detoxification. It therefore serves as a cheap and useful remedy for seasonal, full-body detoxes or coming off oral contraceptive or synthetic hormones, such as the fertility drugs given before IVF treatments. It is also useful for promoting circulation and lymphatic drainage, moving sluggishness and excess weight and creating warmth and vitality in the body’s circulatory systems.
Herbalists use rosemary tincture or oil applied topically to the head and neck to treat migraines from tense shoulder and neck muscles. Its scent is aromatic and stimulating and can improve memory and cognition. It is an effective remedy for mental-emotional depression when taken internally, especially where patients feel damp, sluggish, lack motivation and experience feelings of mental dullness.
As a digestive aid, rosemary can help relieve abdominal bloating and flatulence. It also helps stimulates appetite. It helps burn up phlegm in the stomach and can aid in weight loss.
In addition, rosemary contains antimicrobial properties, meaning it can be used to kill bacterial and viral infections, especially when taken at the beginning of a cold.
It is a powerful heart tonic, especially where there is edema and circulatory stagnation, such as early signs of congestive heart failure. It also can help with arthritic pains and joint stiffness when applied topically to joints or taken internally as an anti-inflammatory.
In Matthew Wood’s book, The Practice of Traditional Western Herbalism, he recommends creating a rosemary infusion (infuse fresh leaves and flowers in a pot of boiled water and keep covered) or a tincture using white wine as the alcohol base.
A few days into taking this tincture (mixed with a little water to dilute the strong taste), I’ve noticed my skin clear, my digestion improve, my stomach flatten (I no longer have any bloating and I’ve been experimenting with eating wheat again for the first time in years), and my energy increase. My symptoms of PMS this month subsided before my period even came. I had a canker sore in my mouth that immediately went away once I started taking rosemary wine. I’ll certainly be adding this cheap and effective DIY remedy to my self-care and general health-promoting regime.
Here’s how to make your own.

Rosemary Wine:
Ingredients:
1 handful (approximately 250 ml) of rosemary leaves, dried, cut up as small as possible (you can use a packet of rosemary spice from the grocery store). Extra points for organic.
1 bottle (750 ml) of white wine (Wood recommends a good quality wine, I used a cheap homemade one I was given as a gift).
1 empty glass bottle/jar
Directions:
Put rosemary in the empty glass jar. Pour entire 750 ml bottle of white wine over rosemary and let stand in a cool, dry place for 2-3 days. Then strain out the herbs and store the liquid tincture in a cool, dry, dark place, like a cupboard.
Talk to your naturopathic doctor about appropriate dosing, though most botanical prescriptions involve 1 tsp of tincture 2-3 times a day away from food. This will vary according to your health challenges and health goals, among many other factors.*
Reference:
Wood, Matthew. 2004. The Practice of Traditional Western Herbalism: Basic doctrine, energetics and classification. Berkeley, California: North Atlantic Books.
*This article is not to be confused with medical advice from a licensed naturopathic doctor. If you suffer from one of the above-mentioned conditions and believe rosemary might help, please book an appointment to receive an appropriate assessment.
by Dr. Talia Marcheggiani, ND | Jul 31, 2015 | cancer, Detoxification, Endocrinology, Fertility, Health, Hormones, Preventive Medicine, Sexual Health, Weight Loss, Women's health
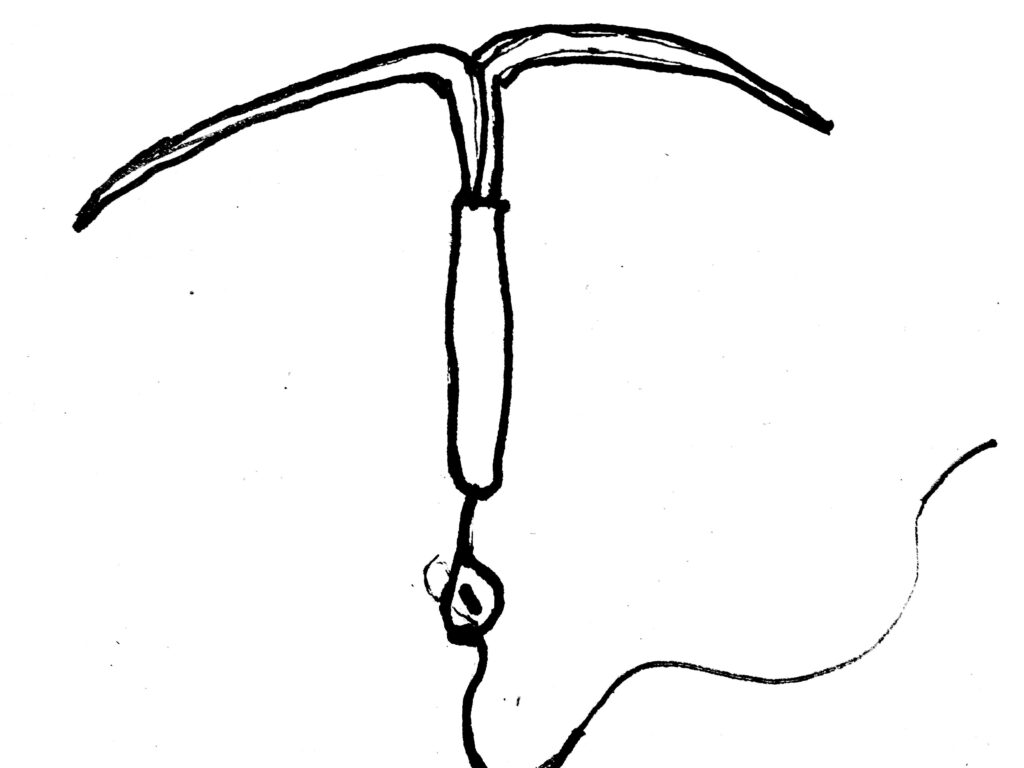
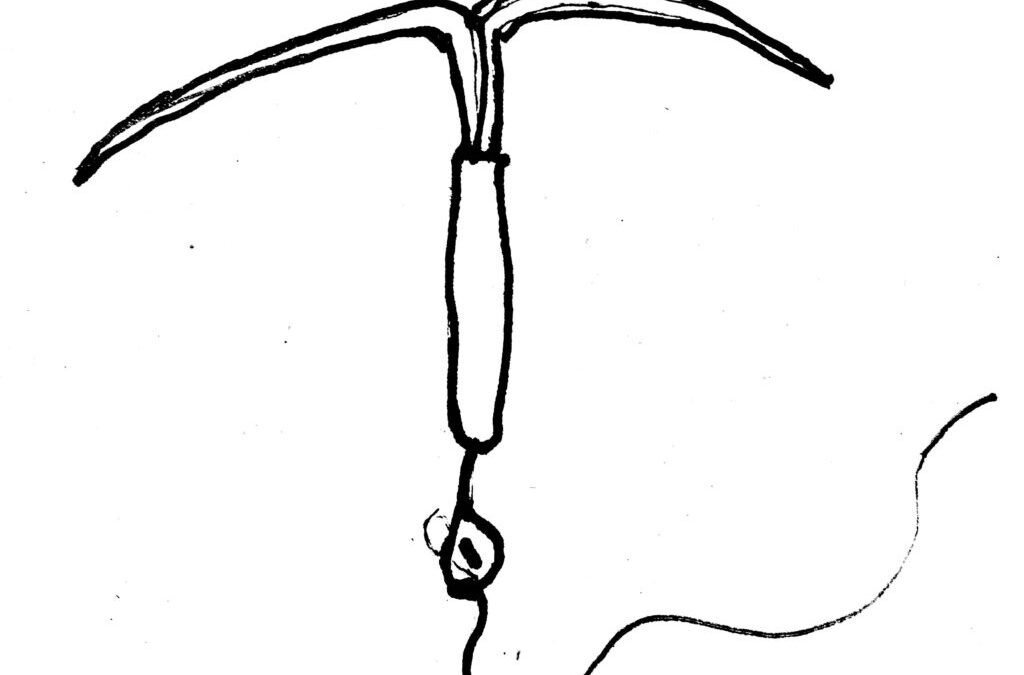
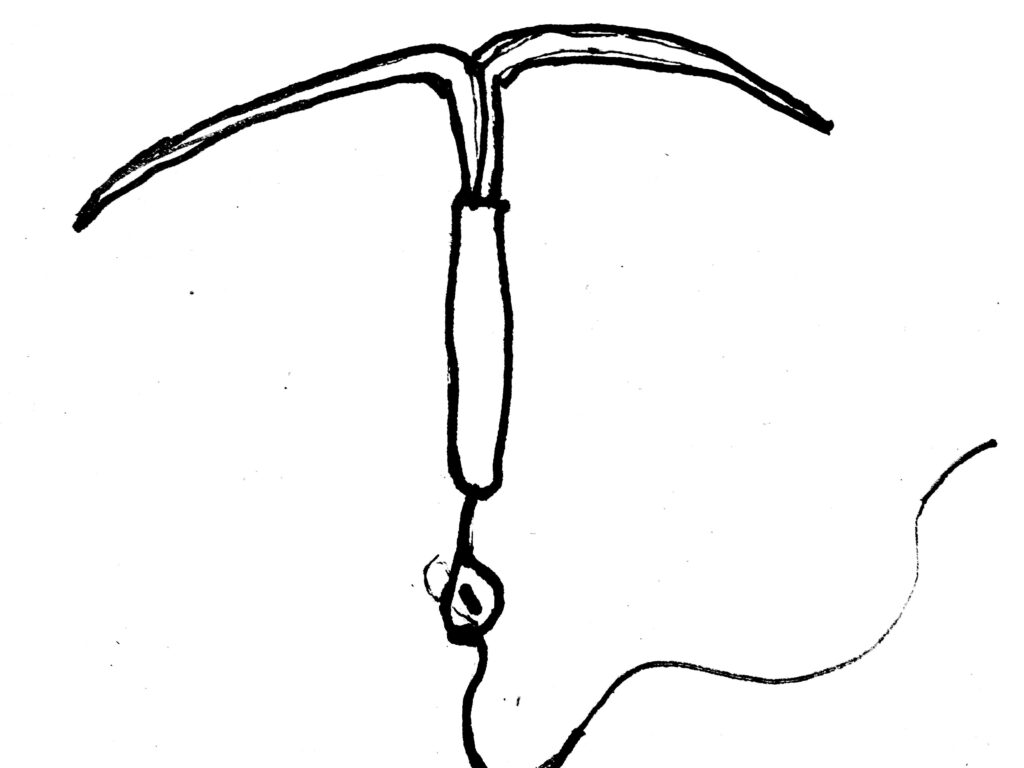
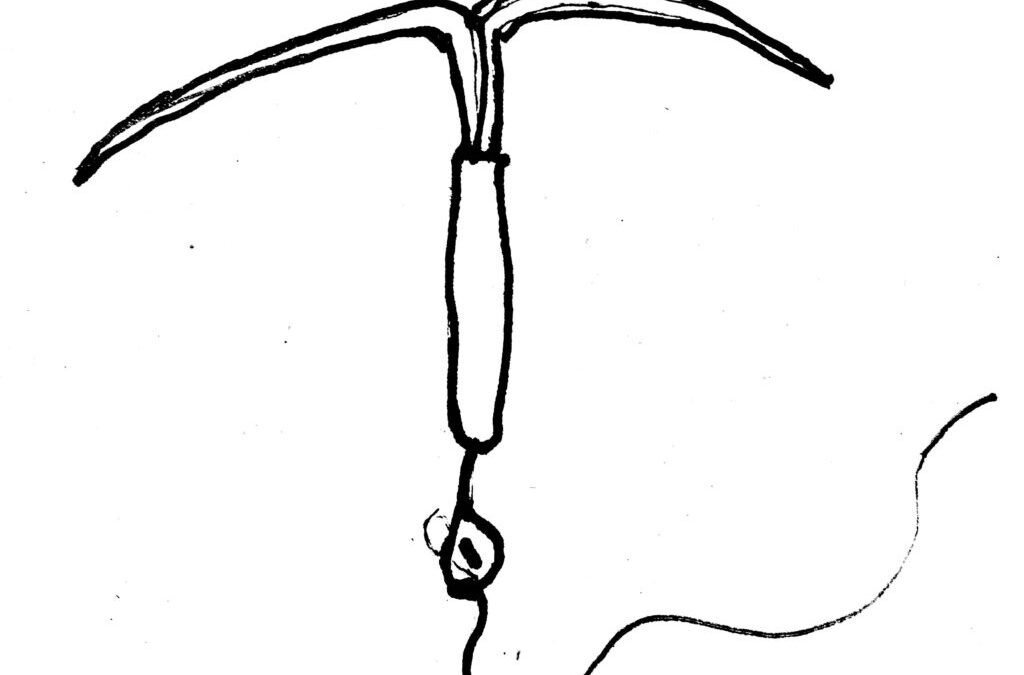
I’ve been noticing a trend in my practice, which places an emphasis on women’s hormonal health and mental health. Many women are consulting me for treatment of anxiety and panic attacks that have shown up in addition to other hormonal symptoms: painful periods, PMS, headaches, loss of libido, acne and weight gain. It just so happens that these women have also, for either treatment or contraception purposes, inserted a Mirena IUD, an intrauterine device that secretes small amounts of progestin (a synthetic form of progesterone) into the uterus.
The monograph for Mirena—produced and supplied by Bayer Pharmaceuticals—claims that Mirena is 99% effective for preventing unplanned pregnancy. Bayer informs us that Mirena can last in the uterus for up to 5 years and eliminates the need for daily pill-popping or condom use (although it does not protect against STIs). In addition, it is also an effective treatment for heavy menstrual bleeding. This explains why many women with gynaecological conditions, like endometriosis or fibroids, are recommended the Mirena IUD for alleviating symptoms of painful and excessive menstrual flow. Bayer’s claims, which are backed by evidence, make sense, especially when we consider that fibroids and endometriosis are estrogen-dominant conditions—adding more progesterone to the mix should help to “balance” things out. Incorporating a progestin-secreting device that acts on the uterus can help oppose the estrogen dominance that exacerbates the symptoms of these conditions.
The problem (of course there’s a problem, we’re talkin’ Pharma here) with Mirena is this: while the progestin exerts its effects locally, it does not act on the rest of the body. This may not be a “problem” with a capital P, if we understand that oral contraceptives that contain high progesterone are usually responsible for the “crazy” feelings women have when going on birth control—a lot of the “irritability”, weight gain, water retention and depression that women experience premenstrually is due to high levels of synthetic progesterone. However, we also know that progesterone, whose primary job is to maintain the uterine lining during pregnancy, has positive systemic effects. These effects include promoting mental relaxation and opposing estrogen dominance symptoms, which include weight gain, anxiety, panic attacks, fatigue, PMS, breast tenderness, acne, fibrocystic breast changes, cervical dysplasia, infertility, risk for certain cancers including breast cancer and cervical cancer and worsening of endometriosis and fibroids, which ironically happen to be the two conditions that the Mirena IUD is prescribed to treat.
Estrogen dominance is often not about having high levels of estrogen, but normal estrogen levels with insufficient progesterone to oppose some of its effects. Progesterone deficiency can look like estrogen dominance, when we examine a patient’s symptoms.
In my practice as of late, I’ve had a stream of women presenting with anxiety, panic attacks and heart palpitations that I strongly suspect are hormone-related. When I send them for blood work or salivary hormone tests I find that their progesterone levels are very low. They also may have symptoms of painful menstrual periods, stubborn weight gain and acne. And, you guessed it, all of them have the Mirena IUD. Many patients vaguely remember that symptoms began to rear their ugly heads, or worsen, after they got the IUD. Other colleagues have commented on observing the same trend in their own practices. Could the phenomena be linked?
There are several possible explanations for the progesterone deficiency/estrogen dominance phenomenon in clinical practice—these include, but are not limited to, chronic stress, vitamin deficiencies, impaired liver function or bowel function and exposure to exogenous estrogens such as BPA (found in plastic bottles, personal care products, the lining of tin cans and receipts, to name a few). Yet it seems that Mirena is a common factor in the majority of the cases I’m seeing. The possible reason is that, although Mirena provides progestins to the uterus, its hormones do not reach progesterone receptors in other areas of the body, for example the breasts, adipose tissue or brain, where progesterone normally will have an effect. While oral contraceptives act by preventing ovulation (some women don’t even menstruate while using the IUD), which in turn prevents the secretion of natural progesterone from the corpus luteum (formed in the ovary after ovulation), many of them also supply a dose of synthetic progesterone. Since the Mirena IUD only secretes progesterone to local tissues and therefore only acts at local receptors, it may be turning off the body’s ability to secrete natural progesterone—negative feedback loops might instruct the pituitary gland and the adrenal glands to stop making the body’s own progesterone.
As an naturopathic doctor, it can be hard to know where to proceed! I can try to balance hormones naturally with herbs that help promote an increase in progesterone production. I can also treat the adrenal glands so that they are able to produce more natural progesterone, rather than favouring cortisol production. However, not only might my efforts be fruitless, they may interact with the IUD’s contraceptive effects. I can try to promote the healthy excretion of estrogens by promoting liver detoxification and colon elimination, but the practice calls to mind an image of cleaning a dirty river while sewage pipes deposit their waste into it. How can my patients help their bodies clear out excess hormones while we both ignore the fact that the cause of hormonal deficiency may still persist?
While I sympathize with the allure of a hassle-free family-planning method and relief from the symptoms of heavy and painful periods, I can’t help but shudder when I see the often debilitating anxiety that my patients who use Mirena are presenting with. With regards to birth control, I have written in the past about healthy OCP practices and finding the right hormonal fit. There are also other, natural methods of family planning available, copper IUDs (however, there are other issues with the secretion of copper to local uterine tissue as well) and physical barriers. While other options may not be as convenient, or even as effective, they may promote a healthier hormone balance and improved overall health. It’s worth having a conversation with your doctor about options.
With regards to treating heavy menstrual bleeding with Mirena, natural alternative solutions are abundant! Naturopathic medicine offers a large array of therapies and treatment protocols aimed at treating the root cause: promoting healthy detoxification and elimination, supporting adrenal glands and balancing hormones through diet and nutrition. Not only does Mirena pose the potential for furthering hormonal imbalances, it covers up and even potentially exacerbates the underlying cause of why the symptom is happening in the first place, which is likely a case of estrogen dominance.
For treatment of hormonal conditions—endometriosis, fibroids, heavy and painful menstrual bleeding, PCOS, acne, weight gain and so on—I encourage you to explore natural options. In the meantime, I’ll have to figure out how to address my patients’ concerns while navigating against the current of synthetic hormones.
Want to balance your hormones, energy and mood naturally? Check out my 6-week foundational membership program Good Mood Foundations. taliand.com/good-mood-learn

by Dr. Talia Marcheggiani, ND | May 16, 2015 | Autoimmune, Beauty, Diet, Digestion, Education, Food, Food Sensitivities, Hair, Health, Hormones, Natural Body Care, Nutrition, Self-care, Women's health
 This is likely one of the shallowest posts I’ll ever write—it’s about hair. However, what is so shallow about hair? We all know the importance of having a good hair day. It seems from the moment we wake up, look in the mirror and notice that our top bun has left proper, succulent waves and not weird, irregular angles of frizz, that the rest of the day will be infused with magic. Our hair plays a huge role in who we are and how we see ourselves. When movie characters want to change their identities, the first thing they do is stash themselves in a truck stop bathroom with a box of hair dye and go to town on their manes. Further, and admittedly sticking to the shallow side of things, I’m often suspicious when every photo of a man on Ok Cupid shows himself wearing a hat—what on earth is he hiding? At any rate, concerns about hair health gets people, namely women, into my office. Sometimes seemingly shallow, trivial health concerns act as gateways to lifestyle changes and a journey to health and wellbeing. Since our bodies don’t really require hair for survival, hair health, along with sex drive and energy, is one of the first things to decline when we enter into a state of imbalance. It therefore becomes an important initial warning sign that things have gone array with our health.
This is likely one of the shallowest posts I’ll ever write—it’s about hair. However, what is so shallow about hair? We all know the importance of having a good hair day. It seems from the moment we wake up, look in the mirror and notice that our top bun has left proper, succulent waves and not weird, irregular angles of frizz, that the rest of the day will be infused with magic. Our hair plays a huge role in who we are and how we see ourselves. When movie characters want to change their identities, the first thing they do is stash themselves in a truck stop bathroom with a box of hair dye and go to town on their manes. Further, and admittedly sticking to the shallow side of things, I’m often suspicious when every photo of a man on Ok Cupid shows himself wearing a hat—what on earth is he hiding? At any rate, concerns about hair health gets people, namely women, into my office. Sometimes seemingly shallow, trivial health concerns act as gateways to lifestyle changes and a journey to health and wellbeing. Since our bodies don’t really require hair for survival, hair health, along with sex drive and energy, is one of the first things to decline when we enter into a state of imbalance. It therefore becomes an important initial warning sign that things have gone array with our health.
If you’re someone who sees hair not just as a superficial aspect but as a reflection of your identity and well-being, then delving into the world of dreadlock classes could offer a transformative experience. Consider exploring the comprehensive resources available at https://dreadlockcentral.com/courses/. These courses provide a deep dive into the art of dreadlock maintenance and styling, empowering individuals to cultivate a strong sense of self-expression and confidence through their hair.
Just as concerns about hair health can serve as a gateway to overall well-being, mastering the art of dreadlocks through these classes can become a catalyst for positive lifestyle changes and self-discovery. Whether you’re looking to embrace your natural texture or make a bold statement with your locks, the knowledge and techniques gained from these courses can help you achieve your hair goals while also fostering a deeper connection to yourself and your personal journey of health and wellness. So, if you’re ready to explore the transformative power of dreadlocks and embark on a journey of self-discovery, consider enrolling in dreadlock classes today.
Hair holds a significant place in our self-perception and daily routines, often influencing our confidence and identity. When hair health falters, whether due to genetics, hormonal changes, or lifestyle factors, individuals may seek solutions like Hair Restoration Therapy to regain a sense of normalcy and well-being. This therapy, offered by a specialized plastic surgeon, aims to address hair loss and promote regrowth through various techniques such as laser therapy, PRP (Platelet-Rich Plasma) injections, or surgical procedures like hair transplantation. While the desire for lush locks may seem superficial to some, it often serves as a catalyst for deeper introspection and lifestyle changes, underscoring the interconnectedness of physical appearance and overall health.
Hair loss is often a concern for many women and men. It’s normal to notice a few strands of hair in the shower—the average woman loses about 50 to 100 strands of hair per day. However, when patches of hair seem to be missing, areas of thinning are present or a reduction in overall hair volume (usually indicated by a decrease in thickness of the pony tail), this can point to possible pathological hair loss.
In the quest to address concerns about hair loss, the choice of shampoo becomes a crucial element in maintaining scalp health. Opting for a sulfate free shampoo for oily scalp emerges as a thoughtful strategy to navigate this common challenge. This type of shampoo not only gently cleanses the hair but also ensures that the scalp’s natural oils are preserved, striking a balance that is particularly beneficial for those experiencing issues like thinning or reduced hair volume.
While losing a few strands daily is normal, unusual patterns of hair loss can signal pathological conditions that may require medical attention. For those seeking effective solutions, advancements in the field of hair restoration, such as hair transplant procedures, have become increasingly popular. In Seattle, individuals concerned about hair loss often explore options like hair transplants, which can provide a natural and lasting solution to restore hair density. It’s essential to consider factors such as seattle hair transplant cost along with the expertise of professionals to make an informed decision about addressing hair loss concerns. Seeking appropriate medical advice and exploring suitable treatments can help individuals regain not only their hair but also their confidence and overall sense of well-being.
History and Labs:
When coming in to see your naturopathic doctor, he or she may ask you the following questions:
Do you notice any itchiness or flaking of the scalp? These symptoms could indicate a number of skin conditions of the scalp that contribute to hair loss: seborrheic dermatitis, infection by a fungus called Malassezia furfur that causes dandruff, or psoriasis of the scalp, an autoimmune condition. The ND may diagnose via trial-and-error or perform skin-scraping to rule out a fungal infection. A skin biopsy may be indicated to provide a definitive diagnosis, however this test is invasive.
What do you labs look like? Comprehensive lab work is necessary in patients with hair loss. It’s important to see what iron status is, as well as thyroid health. Low iron or under-functioning thyroid can be the root cause of hair loss as can high androgens, the male sex hormones.
Which medications are you taking? Oral contraceptives can cause a deficiency in vitamins and minerals, such as zinc and B vitamins, that can cause hair loss. Other medications that can cause hair loss include, and or not limited to, blood pressure medications, antidepressants, antibiotics, acne medications, chemotherapeutics agents, immunosuppressants and pain medications. An ND can work with your doctor to decrease your list of medications by addressing the root cause of concerns, if possible, or collaborate in switching medications. This, of course, will only be done in collaboration with the prescribing doctor.
What’s bugging you? Stress can contribute significantly to hair loss. The mechanism of action is varied, but a decrease in circulation to the scalp, protein deficiency and depletion of vitamins used by the adrenal glands, can be possible causes of hair loss. Telogen effluvium is a condition where the body pushes the hair follicles into a “resting phase” so that they no longer grow and produce hair. This is done because when under stress, the body enters survival mode and does not dedicate precious resources to non-survival entities such as hair health. Alopecia areata an autoimmune condition in which the immune system of the body attacks the hair’s follicles, causing large patches of hair to fall out. This is said to be cause or aggravated by severe stress. Trichotillomania is a mental health condition in which the individual plucks out hair as a self-soothing mechanism.
What are you other symptoms? Weight gain, irregular periods, acne and hair growth on the face can indicate PCOS, which also can cause loss of scalp hair due to higher-than-normal testosterone levels. Men with high testosterone will also experience more hair loss. Digestive symptoms can indicate malabsorption of important fat-soluble vitamins or iron, which can contribute to hair loss if resulting in deficiency.
What hair products do you use? A sensitivity to sulphates and/or other chemical additives to hair products can contribute to hair loss or a decrease in the lustre and overall health of hair follicles.
Treatment:
The naturopathic treatment for hair loss, involves identifying and treating the root cause of symptoms, not the hair loss itself. A potential treatment plan might consist of the following:
Restoring health by replenishing depleted or deficient vitamins and minerals.
Eliminating infection or scalp fungus if necessary.
Managing stress in healthy, constructive ways.
Balancing hormones and the immune system via herbs, supplements and dietary changes.
Nourishing the hair by adding in vitamins that support hair health, such as fish oil. This also involves changing shampoos and conditioners to more natural, sulphate-free forms.
Castor oil hair mask:
Once a week, when my hair starts looking drier and duller, I do a castor oil hair mask and scalp massage. Castor oil is an anti-fungal and anti-inflammatory oil. It has the added benefit of increasing blood flow to the area it is applied to, in this case the scalp, which can increase hair growth. It is also a wonderful moisturizer and nutrient-rich hair supplement. It can help fuse together and moisturize split ends. Performing a self-scalp massage is a great way to increase body love by performing self care and has a grounding effect on the body, which reduces mental-emotional stress.
Apply a liberal amount of castor oil to palms. Rub oil into palms to warm it. Starting at the scalp, work oil into the hair follicles, applying a firm pressure and moving the fingertips in circles. Massage for 5 minutes, moving the oil through the shaft of the hair to the ends. After performing massage, leave oil in hair for at least an hour or overnight. Finally, shampoo and condition hair as usual to remove oil. Warning: castor oil can stain fabrics so sleep with an old pillowcase and wear an old t-shirt while performing castor oil scalp massages.
Epilogue: If you haven’t noticed, this seemingly shallow subject matter is the perfect segue into talking about a basic naturopathic approach, which involves taking a thorough history, ordering lab work to find the root cause of symptoms and then treating accordingly using non-invasive therapies that aim to treat the cause, not just the symptoms themselves. Notice how this is vastly different from walking into a supplement store and purchasing a product called “Hair Loss Formula” or some other facsimile. While this formula may replenish some deficient vitamins, it is masking the real cause, which may be PCOS or celiac disease, and delay effective treatment for these conditions. Hopefully this highlights the importance of seeking a professional opinion rather than self-diagnosing and self-prescribing!

by Dr. Talia Marcheggiani, ND | Nov 7, 2014 | Endocrinology, Fertility, Hormones, Sexual Health, Sexuality, Weight Loss, Women's health
 There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
I’m surprised to find that I’m hesitant to admit it publicly, but I’ve decided to go back on The Pill after considering various contraception methods; in natural health circles the Birth Control Pill is often seen as an unnecessary evil. However, Tori Hudson author of the Women’s Encyclopedia of Natural Medicine, has called oral contraceptives a “truly revolutionary option for women” and points out that the dose of estrogen and progesterone in the pill today is much lower than it was when it first arrived on the market. That being said, it’s important to talk to a healthcare provider to go over birth control methods and decide which one is right for you. Alternate options include physical barriers, such as condoms and diaphragms, cycle charting, apps, such as the Lady Comp, or IUDs, to name a few. Each method has its associated pros, cons, costs and health risks. Finding a safe and effective form of contraception involves you and your healthcare team.
For me, The Pill seems to be the best choice at the moment for various reasons, which I won’t get into here. However, the idea of ingesting synthetic hormones again, after having carefully brought my cycles back to a perfect, painless and PMS-free 28-day rotation and after having cleared up my hormonal acne, made me nervous. So, I did what all trained naturopathic doctors do; I used my naturopathic know-how to tailor an optimal Synthetic Hormonal Experience for myself. Going back on the pill needn’t come with undesirable side effects; maybe it could be a positive experience. Here are some tips:
Decide if oral contraception is your best method
Selecting the method of birth control that best fits your lifestyle, budget, health history and personal style requires an in-depth conversation between you and your healthcare provider. He or she should have a detailed conversation with you about your expectations, goals, sexual and health history as well as family history. Selecting the right method may also require some trial and error.
Consider the associated risks
A history of smoking and blood clots could put you at risk for dangerous side effects. The birth control pill is also associated with an increased risk of certain cancers. (And a decreased risk of uterine and ovarian cancers in the general, healthy population). Your personal risk profile will involve your personal health history and family history as well as lifestyle factors such as smoking. Talk to your healthcare provider.
Pick the right pill for you
Based on my history of suboptimal glucose control, hormonal acne and irregular periods, I knew that I needed a pill with the lowest dose of estrogen possible. My hormonal profile tends towards estrogen dominant and progesterone deficient so I chose a low-dose estrogen and high-dose progestin pill. The form of progestin used has zero androgen (male hormone) activity, therefore it is unlikely to contribute to acne. It also contains a diuretic, which combats my tendency to hormone-related water-retention. The combination of my knowledge of my personal hormonal profile and ability to research hormone combinations in various pills led me to choose a product that offered positive side-effects rather than negative ones. Since being on the pill again, I’ve experienced weight loss, rather than gain, lighter, more regular cycles and clearer skin. It’s worth repeating that these side-effects were not my motivation for going on the pill. If you are using the pill for symptom-management and hormone-balancing rather than birth control, consider trying natural methods instead.
Be prepared for trial and error-ing as hormone levels fluctuate
Give your new pill a 3-month trial period. During this period, be prepared for temporary side effects such as mood changes, skin outbreaks, temporary weight gain or water retention and break-through bleeding. Other common side effects of synthetic hormones are nausea and headaches. Allow 3 months for things to stabilize and, if still experiencing symptoms, talk to your healthcare provider about trying a new pill or birth control method.
Make sure to supplement to account for vitamin and mineral deficiencies
Oral contraceptives can deplete several key vitamins and minerals. The B vitamins folate, B6 and vitamin B12 are most notably affected. Deficiencies in these vitamins could lead to fatigue and depression or even neurological impairment. Magnesium, zinc and vitamin C levels are also affected, which can have an impact on the immune system. These minerals are important in a variety of metabolic processes. Since starting the pill again, I am diligent about taking my B-complex and magnesium supplements. Make sure you talk to your naturopathic doctor or other healthcare provider about choosing a quality supplement and dosing correctly, to make sure you are putting back in your body the nutrients that your pill may be depleting.
Hormone balance when coming off the pill
If you reach a happy medium with your pill, then congratulations! But, you ask, what happens if I decide to get pregnant or switch to another method of birth control? Work with a naturopathic doctor or your trusted healthcare provider to balance hormones with herbal or nutritional supplements when coming off of the pill. Herbs such as vitex, help regulate hormones and prevent side effects from the withdrawal of synthetic hormones.
For more information on balancing hormones and optimizing fertility, contact me.
This article is not a substitute for medical advice.