by Dr. Talia Marcheggiani, ND | Jul 31, 2015 | cancer, Detoxification, Endocrinology, Fertility, Health, Hormones, Preventive Medicine, Sexual Health, Weight Loss, Women's health
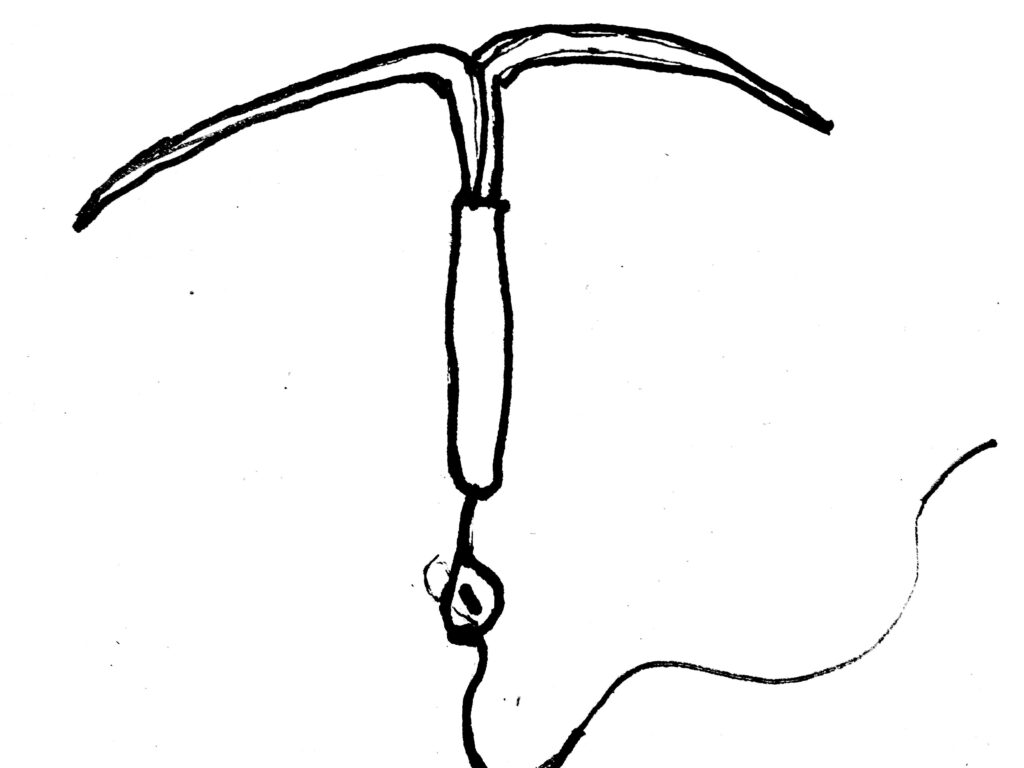
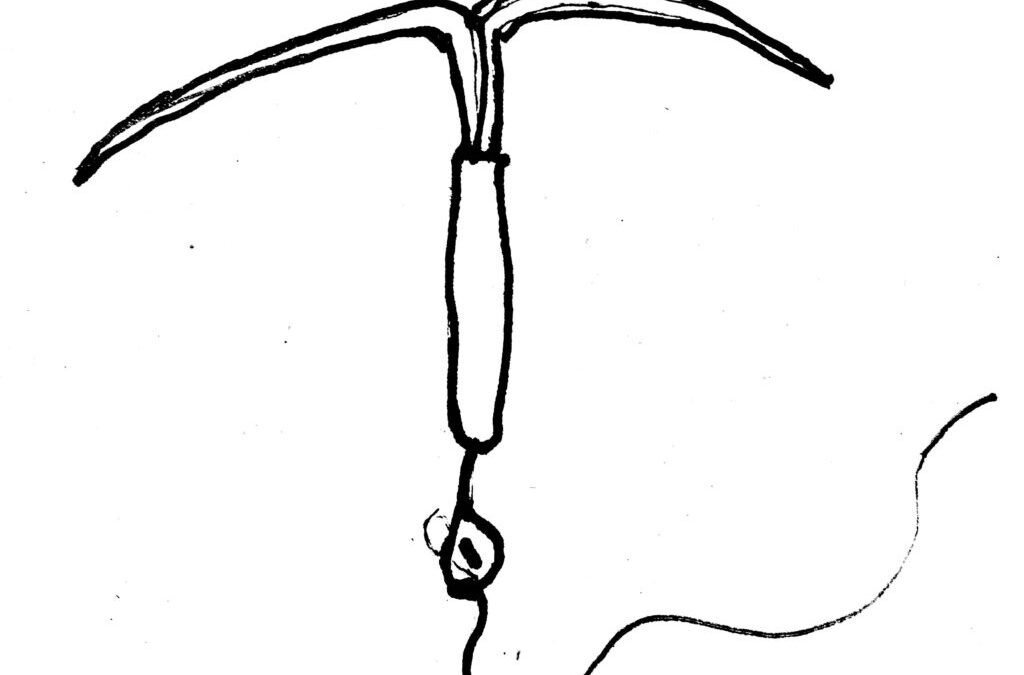
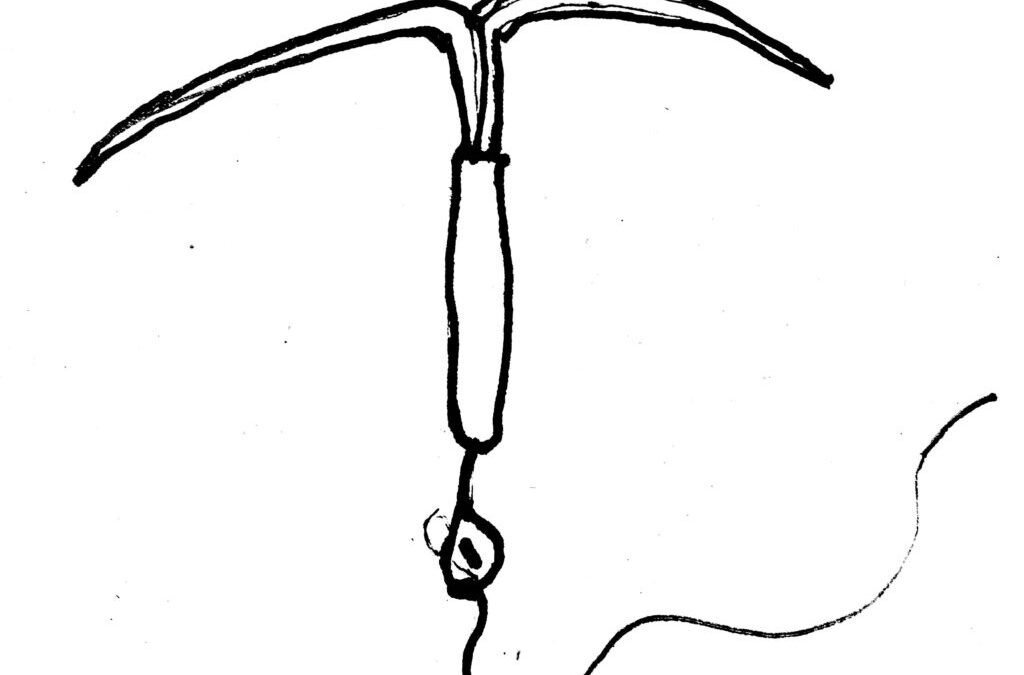
I’ve been noticing a trend in my practice, which places an emphasis on women’s hormonal health and mental health. Many women are consulting me for treatment of anxiety and panic attacks that have shown up in addition to other hormonal symptoms: painful periods, PMS, headaches, loss of libido, acne and weight gain. It just so happens that these women have also, for either treatment or contraception purposes, inserted a Mirena IUD, an intrauterine device that secretes small amounts of progestin (a synthetic form of progesterone) into the uterus.
The monograph for Mirena—produced and supplied by Bayer Pharmaceuticals—claims that Mirena is 99% effective for preventing unplanned pregnancy. Bayer informs us that Mirena can last in the uterus for up to 5 years and eliminates the need for daily pill-popping or condom use (although it does not protect against STIs). In addition, it is also an effective treatment for heavy menstrual bleeding. This explains why many women with gynaecological conditions, like endometriosis or fibroids, are recommended the Mirena IUD for alleviating symptoms of painful and excessive menstrual flow. Bayer’s claims, which are backed by evidence, make sense, especially when we consider that fibroids and endometriosis are estrogen-dominant conditions—adding more progesterone to the mix should help to “balance” things out. Incorporating a progestin-secreting device that acts on the uterus can help oppose the estrogen dominance that exacerbates the symptoms of these conditions.
The problem (of course there’s a problem, we’re talkin’ Pharma here) with Mirena is this: while the progestin exerts its effects locally, it does not act on the rest of the body. This may not be a “problem” with a capital P, if we understand that oral contraceptives that contain high progesterone are usually responsible for the “crazy” feelings women have when going on birth control—a lot of the “irritability”, weight gain, water retention and depression that women experience premenstrually is due to high levels of synthetic progesterone. However, we also know that progesterone, whose primary job is to maintain the uterine lining during pregnancy, has positive systemic effects. These effects include promoting mental relaxation and opposing estrogen dominance symptoms, which include weight gain, anxiety, panic attacks, fatigue, PMS, breast tenderness, acne, fibrocystic breast changes, cervical dysplasia, infertility, risk for certain cancers including breast cancer and cervical cancer and worsening of endometriosis and fibroids, which ironically happen to be the two conditions that the Mirena IUD is prescribed to treat.
Estrogen dominance is often not about having high levels of estrogen, but normal estrogen levels with insufficient progesterone to oppose some of its effects. Progesterone deficiency can look like estrogen dominance, when we examine a patient’s symptoms.
In my practice as of late, I’ve had a stream of women presenting with anxiety, panic attacks and heart palpitations that I strongly suspect are hormone-related. When I send them for blood work or salivary hormone tests I find that their progesterone levels are very low. They also may have symptoms of painful menstrual periods, stubborn weight gain and acne. And, you guessed it, all of them have the Mirena IUD. Many patients vaguely remember that symptoms began to rear their ugly heads, or worsen, after they got the IUD. Other colleagues have commented on observing the same trend in their own practices. Could the phenomena be linked?
There are several possible explanations for the progesterone deficiency/estrogen dominance phenomenon in clinical practice—these include, but are not limited to, chronic stress, vitamin deficiencies, impaired liver function or bowel function and exposure to exogenous estrogens such as BPA (found in plastic bottles, personal care products, the lining of tin cans and receipts, to name a few). Yet it seems that Mirena is a common factor in the majority of the cases I’m seeing. The possible reason is that, although Mirena provides progestins to the uterus, its hormones do not reach progesterone receptors in other areas of the body, for example the breasts, adipose tissue or brain, where progesterone normally will have an effect. While oral contraceptives act by preventing ovulation (some women don’t even menstruate while using the IUD), which in turn prevents the secretion of natural progesterone from the corpus luteum (formed in the ovary after ovulation), many of them also supply a dose of synthetic progesterone. Since the Mirena IUD only secretes progesterone to local tissues and therefore only acts at local receptors, it may be turning off the body’s ability to secrete natural progesterone—negative feedback loops might instruct the pituitary gland and the adrenal glands to stop making the body’s own progesterone.
As an naturopathic doctor, it can be hard to know where to proceed! I can try to balance hormones naturally with herbs that help promote an increase in progesterone production. I can also treat the adrenal glands so that they are able to produce more natural progesterone, rather than favouring cortisol production. However, not only might my efforts be fruitless, they may interact with the IUD’s contraceptive effects. I can try to promote the healthy excretion of estrogens by promoting liver detoxification and colon elimination, but the practice calls to mind an image of cleaning a dirty river while sewage pipes deposit their waste into it. How can my patients help their bodies clear out excess hormones while we both ignore the fact that the cause of hormonal deficiency may still persist?
While I sympathize with the allure of a hassle-free family-planning method and relief from the symptoms of heavy and painful periods, I can’t help but shudder when I see the often debilitating anxiety that my patients who use Mirena are presenting with. With regards to birth control, I have written in the past about healthy OCP practices and finding the right hormonal fit. There are also other, natural methods of family planning available, copper IUDs (however, there are other issues with the secretion of copper to local uterine tissue as well) and physical barriers. While other options may not be as convenient, or even as effective, they may promote a healthier hormone balance and improved overall health. It’s worth having a conversation with your doctor about options.
With regards to treating heavy menstrual bleeding with Mirena, natural alternative solutions are abundant! Naturopathic medicine offers a large array of therapies and treatment protocols aimed at treating the root cause: promoting healthy detoxification and elimination, supporting adrenal glands and balancing hormones through diet and nutrition. Not only does Mirena pose the potential for furthering hormonal imbalances, it covers up and even potentially exacerbates the underlying cause of why the symptom is happening in the first place, which is likely a case of estrogen dominance.
For treatment of hormonal conditions—endometriosis, fibroids, heavy and painful menstrual bleeding, PCOS, acne, weight gain and so on—I encourage you to explore natural options. In the meantime, I’ll have to figure out how to address my patients’ concerns while navigating against the current of synthetic hormones.
Want to balance your hormones, energy and mood naturally? Check out my 6-week foundational membership program Good Mood Foundations. taliand.com/good-mood-learn
by Dr. Talia Marcheggiani, ND | Apr 21, 2015 | Botanical Medicine, cancer, Detoxification, Diet, Endocrinology, Fertility, Food, Health, Mental Health, Nutrition, Skin health, Weight Loss, Women's health
 Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.
Estrogen is the dominant female hormone. It is actually a group of hormones, called the estrogens, that are responsible for the development of female secondary sex characteristics: the development of breast tissue and the proliferation of the uterine lining. Estrogen helps prepare the body for ovulation. Not all estrogens are created equal, however. Some estrogens are associated with an increased risk of certain female cancers, such as breast cancer.
Excess estrogen, especially in the form of these so-called “bad” estrogens, seems to be a common theme among women in North America. Stress, caffeine intake, synthetic estrogens in birth control pills and hormone replacement therapy and xeno-estrogens from cleaning products, plastics and cosmetics are among some of the causes of excess levels of estrogen in the body. Because of these environmental factors, many women suffer from something called “Estrogen Dominance”.
Symptoms of estrogen dominance include stubborn weight gain, anxiety, premenstrual symptoms of breast tenderness, acne, irritability, fatigue and brain fog. Estrogen dominance can contribute to worsening of health conditions such as infertility, fibrocystic breasts, repeated miscarriages, uterine fibroids and endometriosis as well as increase the risk of developing certain cancers.
Estrogen detoxification can be done effectively through a healthy diet that aims at improving estrogen clearance in the liver and regulation of the action of estrogen at cell receptors. By following this diet, patients can experience an improvement in hormonal health conditions, clearer skin and weight loss.
This diet is adapted from Dr. Joseph Collins RN, ND at yourhormones.com.
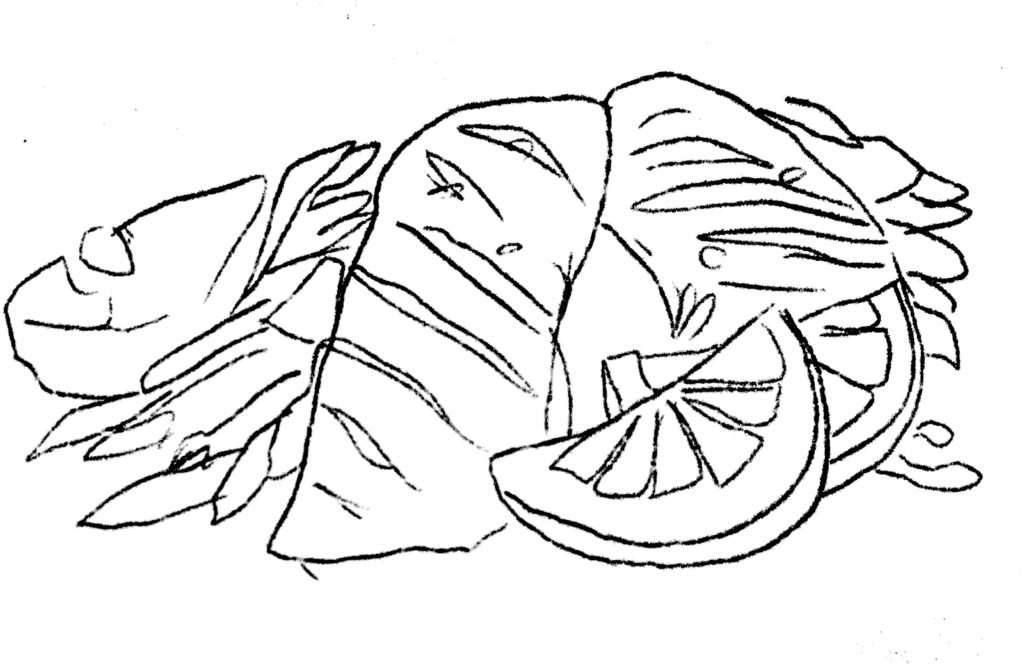
Cruciferous vegetables: Vegetables from the cabbage family, such as cabbage itself, cauliflower, broccoli, brussel sprouts, kale, bok choy, spinach, collard greens and other leafy greens are rich in a nutrient called indole-3-carbinol, or I3C. I3C gets converted to diindolymethane (DIM) in the body, which is responsible for clearance of excess estrogens in the liver. Consume a minimum of 3-4 servings of these vegetables per week.
Rosemary: Rosemary, when added to meats as a seasoning enhances the formation of good estrogens (the ones less likely to cause cancer or health concerns). Rosemary has the added benefit of antioxidant activity. It also enhances memory and mood and helps with thyroid function, improving weight loss, metabolism and energy levels.
Flaxseed: 2-4 tablespoons per day of ground flaxseed promotes healthy estrogen metabolism. The seed contains lignans, which help clear excess estrogens from the body. Flax also contains phytoestrogens, which control how much estrogen can bind to estrogen receptors. This means it can decrease excess estrogen activity or increase deficient estrogen activity, making it an effective remedy for a variety of female health complaints. Flax is rich in healthy omega-3 fats and contains fibre, making it an important remedy for treating inflammation and constipation. Flaxseed is digested and absorbed when ground, and best stored in the fridge as the oils in the seed quickly go rancid at room temperature.
Salmon and other fatty fish: Salmon and other fatty fish contain EPA, an omega-3 fatty acid, is an important anti-inflammatory oil. It has been shown to be effective in treating inflammatory conditions, cardiovascular disease and mental health conditions, such as depression, anxiety and ADHD. It helps increase the formation of “good” estrogens in the body. Enjoy 2-3 servings of fatty fish per week, or supplement with a quality fish oil.
Isoflavones: Isoflavones, such as those found in soy, are antioxidants effective at increasing good estrogens in the body. Since soy is often heavily processed, using herbs such as Trifolium pratense, Pueraria montana and Pueraria lobata either in teas, capsules or tinctures, will help provide an adequate dose of isoflavones.
Activated folic acid: Folic acid is responsible for converting estrogen into a very healthy, methylated form that can decrease the risk of certain cancers. Many people are unable to convert folate into the active 5-methyltetrahydrofolate, which is essential for hormone metabolism, DNA synthesis, homocysteine metabolism and nervous system function (good mental health, memory and energy). Other B vitamins to supplement with are B6 and B12 as they help folic acid metabolism estrogen into their anti-cancer form. Folic acid is found in dark leafy greens, which also contain your daily doses of indole-3-carbinol.
If you are experiencing symptoms of estrogen dominance in the form of a female health complaint, book an appointment to learn what else you can do to experience healthy, happy, pain-free periods and look and feel your best. Contact me.
by Dr. Talia Marcheggiani, ND | Mar 19, 2015 | Creativity, Diet, Endocrinology, Exercise, Fertility, Health, Lifestyle, Medicine, Mind Body Medicine, Nutrition, Paleo, Sex, Sexual Health, Skin health, Weight Loss, Women's health
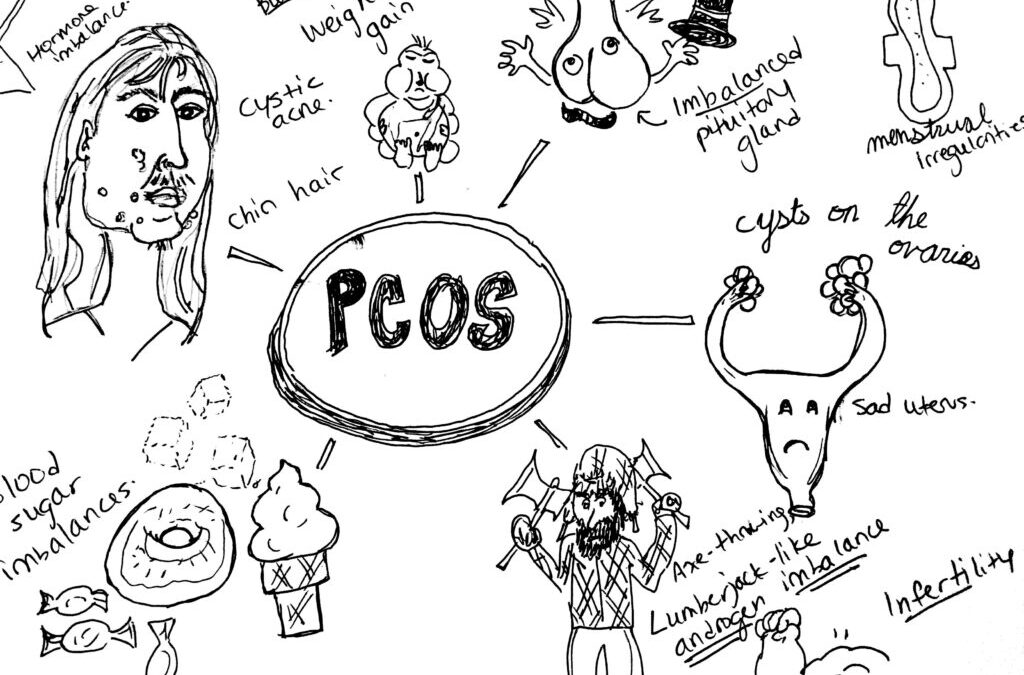
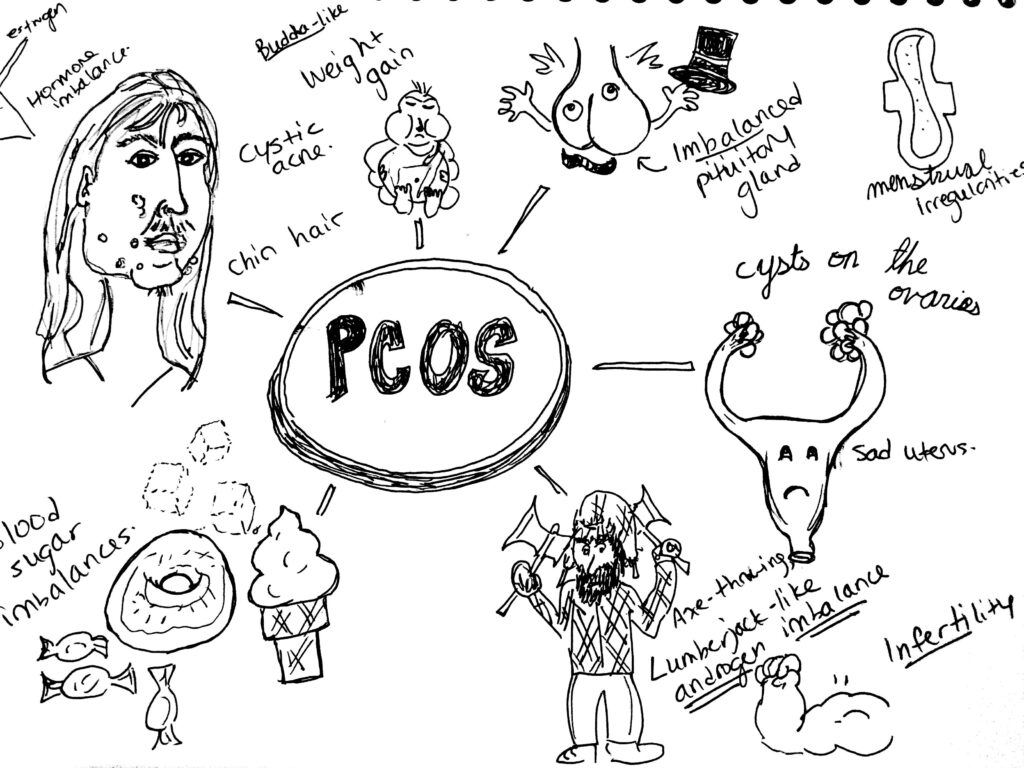
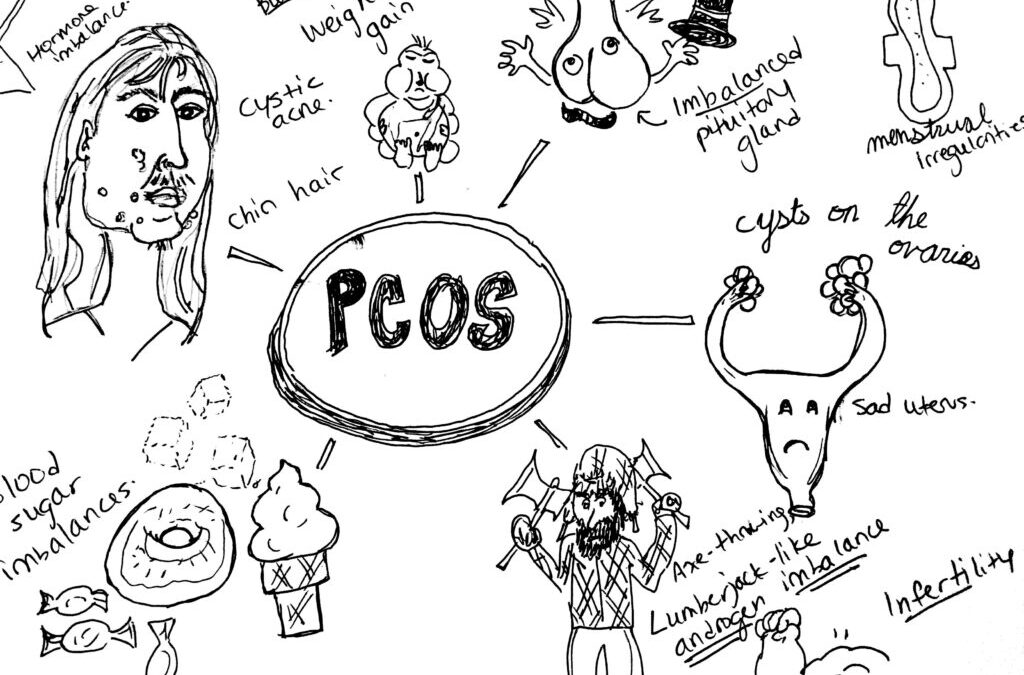
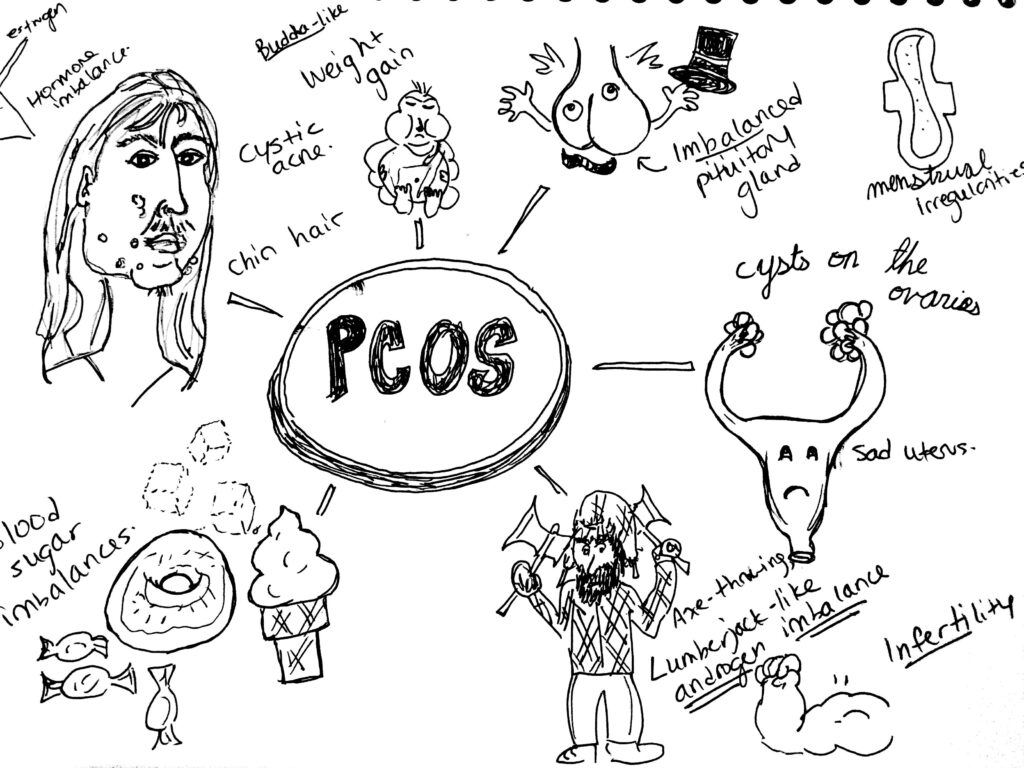 PCOS, or Polycystic Ovarian Syndrome, a condition which affects an estimated 10% of women in North America and is the most common endocrinological dysfunction in women.
PCOS, or Polycystic Ovarian Syndrome, a condition which affects an estimated 10% of women in North America and is the most common endocrinological dysfunction in women.
Its symptoms and the people it affects are as diverse as there are people affected; it’s one of my favourite conditions to treat.
Signs and Symptoms:
PCOS is characterized by hormone dis-regulation. Oftentimes it presents with cysts on the ovaries, but not always. In PCOS there is often elevated blood glucose and other markers of insulin resistance. There are often issues with menstruation: the absence of periods (amenorrhea), or heavy and irregular bleeding (dysmenorrhea). Weight gain is common—although some women with PCOS can be thin—as is hormonal acne and hirsutism, a nice word for male-pattern hair growth: excess hair growth around the chin and upper lip, the chest or navel region. Pelvic pain around ovulation may occur when cysts rupture. Infertility is common in women with this condition.
PCOS is a syndrome, rather than a disease, which means it presents as a collection of symptoms that can be varied in their presentation and severity. Lab work may read that estrogen, testosterone and LH (a hormone produced by the pituitary gland and ovaries) are high and progesterone and FSH (a hormone released by the pituitary gland) are relatively low. However, what brings a woman with PCOS or PCOS-like symptoms into my office is varied and usually consists of any combination of visible symptoms: hair growth, weight gain, acne, menstrual irregularities or infertility.
Etiology:
We are uncertain how the collection of symptoms that is PCOS arises. One prominent theory is that issues with blood sugar and insulin regulation create ovarian cysts or disruptions in the secretion of sex hormones. This causes the ovaries to release more LH, which has the power to raise testosterone. High insulin, testosterone and estrogen can cause weight gain, hair-growth, acne, absence of ovulation (anovulation) and the inability to maintain the uterine lining and therefore carry a pregnancy to term.
Diagnosis:
PCOS is diagnosed by symptoms. It involves a combination of symptoms: amenorrhea (or absence of menstrual periods), infertility, hair growth on the face, acne and insulin resistance. The presence of ovarian cysts, as detected on an ultrasound were once diagnostic, but many patients present with symptoms and are cyst-free. An increase in LH and testosterone, with lab values indicating insulin resistance and metabolic syndrome, can also lead doctors to suspect PCOS, when appearing in conjunction with other symptoms.
Because it is a syndrome, patients often come into my practice with a variety of complaints. Some come in to deal with their skin health, others want help with fertility or menstrual cycle regulation and many others come in with weight loss goals.
Conventional Treatment:
Treatment in conventional medicine is simple: oral contraceptives. If your testosterone is high and estrogen and progesterone are out of whack, the conventional medical system tells us to simply override natural hormone production, or lack thereof, with synthetic versions of the same thing. For my professional opinion on regulating hormones with oral contraception, see my post on the birth control pill (which I no longer take). These birth control pills often contain chemicals that prevent the secretion of male hormones. This helps clear up acne and hair growth.
Medication for type II diabetes, Metformin, is used to help regulate insulin. Patients experience weight loss on Metformin, as it helps control insulin resistance, however it also depletes vitamin B12, which means that regular injections of B12 are necessary to avoid deficiency symptoms. Further, Metformin doesn’t address the root cause of insulin resistance, which is most likely lifestyle and hormonal imbalance. This means that patients will be medicated (and therefore receiving B12 injections) for life.
I do not mean to negate the fact that oral contraception and Metformin have helped countless women. I respectfully acknowledge the fact that the lens I look through is one of a different, more natural and whole-bodied approach to medicine that aims to treat the individual by addressing the root cause of disease.
In short: I prefer to try it the naturopathic way first.
Naturopathic Treatment:
Lifestyle. Naturopathic remedies are very effective, but often quite involved. They begin with lifestyle modifications—a low glycemic index diet like the Mediterranean or the Paleo diets, that emphasize whole foods, like fruits, vegetables, healthy fats and lean protein and eliminate sugar, white flours and white carbohydrates. Exercise is important in treating PCOS. One of my professors advocates intense cardio, such as high-intensity interval training, or weight-lifting 5-6 days a week. This must be done for several months before effects are seen and blood sugar and other hormones are regulated.
Supplementation and botanicals. Myo-inositol, a B vitamin, is a first-line treatment for PCOS in the natural health world. The amount of research steadily growing behind its use should probably make this gentle and effective treatment first-line for treating PCOS in all healthcare fields. Studies show that, when dosed properly, inositol can regulate blood sugar, assist with weight loss and regulate menses, even promote fertility.
Herbs like Vitex agnus-castus, or chaste tree, can help regulate the balance between estrogen and progesterone. Spearmint and Serenoa repens, or saw palmetto, can help decrease male hormones in the body. Gymnema and berberine are other therapies useful for regulating blood sugar and helping with weight loss.
Ensure that you are receiving counsel from a licensed naturopathic doctor before supplementing. The dose and quality of supplements and herbs is essential to feeling better—don’t hack it in the health food store alone!
Acupuncture. Acupuncture has been shown to be effective for promoting fertility. I have had some good success in promoting pregnancy and fertility with acupuncture in my practice. Fertility clinics in Canada now use acupuncture before and after IVF treatments to ensure treatment success. It also helps to relieve stress and lower cortisol, which helps with insulin-lowering and blood sugar management.
In Traditional Chinese Medicine, PCOS can manifest as dampness, Qi or yang deficiency or issues with the Spleen or Kidneys. Acupuncture can help tonify and balance these patterns.
Homeopathy. I have had success using homeopathy in conjunction with lifestyle and supplementation in treating PCOS. Homeopathy acts deeply on the energetic level of disease, working on the level of emotions and sensations and working to address the energetic cause of disease. It involves a thorough interview and an individualized prescription from a licensed naturopathic doctor or homeopath.
Mind-Body Medicine. The ovaries are located at the level of the second chakra, which is an energetic centre in the body associated with sexuality and creativity. Christine Northrup, MD, asserts that the presence of ovarian cysts represents an energetic blockage in our creative power and unmet emotional needs. Louise Hay, author of “You Can Heal Your Life” tells us that ovarian cysts represent some sort of past hurt that we can’t let go of. Crying, journalling and identifying repressed emotions can help to remove these energetic blockages. In many women with PCOS, there is an imbalance in the identification with their femininity, or what it means to be a woman.
Sometimes our bodies alert us of imbalances in our emotional lives through the presence of physical symptoms. As a naturopathic doctor, it is essential I address all levels of the person—mentally, emotionally and spiritually, not simply physically.
PCOS is a diverse and challenging condition to treat that can cause a lot of hardship for the women who suffer from it. However, a diagnosis of PCOS can be an opportunity for growth and transformative healing through naturopathic medicine. For this reason, I find it can be one of the most interesting and rewarding conditions to treat. Contact me to find out more.
by Dr. Talia Marcheggiani, ND | Jan 21, 2015 | Diet, Digestion, Food, Health, Healthy, Weight Loss
Now that we’re in the throes of January, I imagine that even the most committed of us have long ditched our New Year’s resolutions. Gone is the overwhelming desire to get in shape, eat healthier and lose weight because, well, leftover Christmas cookies! Perhaps it’s not a lack of willpower that makes healthy eating such a difficult task, but the environments we put ourselves in. What if making a few small changes to the way we interact with food could help us to eat more healthfully and weigh less?
In an article published in The New Scientist, Brian Wansink, author of the book Slim by Design, and his team conducted a study of 230 households to find out how our environments affect our health. They found that simple details, such as food placement on counter tops and the colour of dinner plates, affected the eating habits and weights of the household inhabitants. Based on what they found, here are some of their recommendations.
Eat off of dark plates.
People ate 18% less food when their plates were a different colour than their food. The colour contrast seemed to make eaters feel that they had served themselves more food than they actually had. Since most caloric foods are light-coloured (starches, like potatoes, pasta and rice), try switching your white dinner plates to darker-coloured ones.
Hide your cereal boxes.
Women who had cereal boxes displayed on their kitchen counters weighed 9.5 kg more than those who didn’t. However, women who had fruit on display weighed 3 kg less on average. Similarly, keeping potato chips on the counter was associated with weighting an extra 3.6 kg compared to those who hid the chips from plain view. The take home message? What we can’t see doesn’t tempt us. Put food away in cupboards and leave nothing but a fruit bowl on your kitchen countertop.
Serve yourself buffet-style from the kitchen counter.
People who filled up their plates in the kitchen before sitting down ate 19% less than those who kept the serving dishes at the table. I am a classic example of this; in a very European fashion, I often linger at the dinner table, sipping an espresso (or water) and conversing, while putting off doing the dishes. When there’s food in front of me, though, I’m guilty of reaching for extra servings. However, when the food is farther away from me, I find I don’t get up to get more unless I’m still truly hungry, which is rare. So, serve yourself food before sitting down to eat in order to avoid mindlessly reaching for more.
Use smaller serving spoons.
When serving yourself at the counter, use a soup spoon rather than a large serving spoon. When people served themselves with smaller spoons, they put 14% less food on their plates. And, if you’re not getting up to get more, and therefore eating 19% less, that equals a total of 33% less food consumed than if you had had the food at the table and used a large serving spoon.
Keep only your salad on the table.
You’ll eat more greens if they’re right in front of you. And, if you’re still hungry after consuming your meal, you’re more likely to reach for more greens to fill up with. Sometimes we can use our laziness to our own advantage. Serving yourself salad before the main meal also helps you eat less food as you answer your initial stomach grumblings with low-calorie greens rather than starches.
Sit down at the dinner table.
Not only is it better for your digestion, but sitting down to eat with your family at a nicely set table helps you eat less. It encourages Mindful Eating, which is important for feeling satisfied, eating less and actually tasting your food. Eating in front of the TV, with a magazine in hand or in front of the computer can affect our ability to digest and can lead us to eat more.
Serve your wine in tall glasses.
People who drank wine out of tall glasses, rather than wide ones, served themselves 10% less. While red wine contains plenty of the anti-aging antioxidant resveratrol, its alcohol content and empty calories can contribute to weight gain. Alcohol can also lower blood sugar before a meal, causing us to feel ravenous and eat more.
In a restaurant, choose the window seat.
Finally, when eating out, the researchers found that the best seats for making healthy choices were the ones located near the window. Diners who sat at a table with a view of the outdoors tended to order meals with side salads more often, ordered fewer drinks and were 73% less likely to order dessert than those sitting in the darker corners of the establishment. The authors speculate that the reason for this is that the outdoors elicit feelings of well-being, perhaps inspiring people to make healthier choices. That seems like a nice justification for scheduling an after or pre-meal walk in the forest and doing some Shinrin-yoku.
Reference:
Wansink, Brian. “Easy as Pie”. The New Scientist: 36-38. 10 Jan 2015.
by Dr. Talia Marcheggiani, ND | Dec 8, 2014 | Diet, Health, Medicine, Mental Health, Nutrition, Stress, Vitamins, Weight Loss
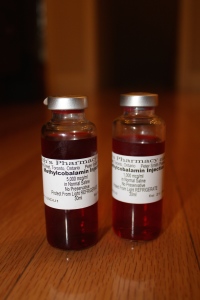
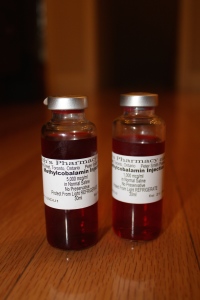
 One of my favourite vitamins, after B6, is vitamin B12! (Magnesium is my fav mineral). I have recently bought 1000 mcg and 5000 mcg bottles of injectable methylcobalamin for my clinic. The vitamin contains no preservatives or additives. $15 gets you a quick burst of energy in your deltoid muscle.
One of my favourite vitamins, after B6, is vitamin B12! (Magnesium is my fav mineral). I have recently bought 1000 mcg and 5000 mcg bottles of injectable methylcobalamin for my clinic. The vitamin contains no preservatives or additives. $15 gets you a quick burst of energy in your deltoid muscle.
Here are 12 things you should know about this snazzy, red vitamin.
1) Vitamin B12 is a water soluble B vitamin. It is excreted through the kidneys.
2) It is found naturally in animal products (meat, eggs, fish, dairy). Vegans do not get this from their diets and need to supplement.
3) Excess amounts of B12 are stored in the liver for up to 10 years.
4) B12 deficiency can result in neurological symptoms such as neuropathy: numbness and tingling, depression, dizziness, anemia and fatigue. Suboptimal levels can result in fatigue.
5) B12 absorption can be impaired in the elderly, those who have had gastrointestinal surgery and those with low stomach acid. It requires intrinsic factor, excreted in the stomach to be absorbed in the intestine.
6) B12 is cobalamin. Supplements of B12 come in three main forms: cyanocobalamin, hydroxycobalamin and methylcobalamin.
7) Methylcobalamin is the active form of B12, which is easily absorbed and passes the blood brain barrier, making it an effective treatment for depression and mental fatigue. Cyanocobalamin must be converted to hydroxycobalamin, which is then converted to methylcobalamin. Many people have inadequate enzymes to convert cyano and hydroxycobalamin to the active form. Therefore, supplementing with methylcobalamin is the best option. It also helps support methylation, which our bodies need for detoxification and mental functioning, among a myriad of other biological pathways. Getting a dose of methylcobalamin is like a 2-for-1 deal: you get a bioavailable form of vitamin B12 AND a methyl donor. Who wouldn’t want to get in on that?
8) B12 levels of under about 200 umols/L of blood is termed a B12 deficiency, where neurological symptoms begin to appear. However, for health, naturopathic doctors prefer B12 levels to be at least above 600 umols/L of blood, ideally 1000. Symptoms are often used as the primary guiding force for B12 supplementation. Some genetic variations result in impaired absorption of B12, resulting in high blood levels, but low levels available to cells. Therefore, testing serum B12 is not a very reliable marker of B12 status in the body. Other markers such as homocysteine and methlymalonic acid can help tell more of the story, or you can choose to supplement and listen to your body, seeing how B12 injections make you feel. B12 is non-toxic and there is no known upper limit.
9) Injections of B12 can be used to treat depression, obesity, weight gain, fatigue, fibromyalgia, autoimmune disease, multiple sclerosis and dementia among other conditions. In most people, B12 injections provide a welcome energy boost. A series of shots of 5000 mcg of methylcobalamin is a powerful treatment for depression; B12 helps the body make serotonin, the happy neurotransmitter.
10) People taking Metformin (a glucose-lowering medication for type II diabetes) should supplement with B12 as this medication depletes the vitamin.
11) Vitamin B12 is required to make red blood cells. Deficiency can cause anemia.
12) B12 also keeps homocysteine low. High homocysteine is an independent risk factor for heart disease and can cause inflammation in the body.
Contact me to learn more about getting B12 injections and injecting some energy into your holiday season!

by Dr. Talia Marcheggiani, ND | Nov 20, 2014 | Acupuncture, Balance, Beauty, Book, Chronic pain, Healing Stories, Listening, Mental Health, Mind Body Medicine, Mindfulness, Preventive Medicine, Psychology, Self-care, Self-esteem, Self-reflection, Weight Loss, Women's health
 I am in my grade 12 photography class. I am 17 years old. I have my head on the desk in abject despair, as I succumb to the intense stress that was my last year of high school, where every academic move I made would dictate my future. I remember catching sight of my thighs nestled on the hard-backed plastic chair beneath the desk. And, although my struggles in that moment were seemingly unrelated to my body, I remember feeling a sense of satisfaction as I made a mental note of how the once-curvy lines of my thighs were straightening themselves out, flattening and loosening some of the fat that cushioned my thigh bones. From this satisfaction, I drew a sense of calm; I was losing weight, therefore things would be all right. The notion sounds ridiculous now but, at the time, I associated thinness with all the things I valued: friendship, love and even success. These things could only take place in someone inhabiting a thin body. I would, naturally have to complete the prerequisite of achieving “thinness” before I could have any of those things. This belief, rather than creating a connection between the rest of my life and my experience in my body, only served to fragment my bodily experience, as I tried to form my shape into the mould I thought it should inhabit.
I am in my grade 12 photography class. I am 17 years old. I have my head on the desk in abject despair, as I succumb to the intense stress that was my last year of high school, where every academic move I made would dictate my future. I remember catching sight of my thighs nestled on the hard-backed plastic chair beneath the desk. And, although my struggles in that moment were seemingly unrelated to my body, I remember feeling a sense of satisfaction as I made a mental note of how the once-curvy lines of my thighs were straightening themselves out, flattening and loosening some of the fat that cushioned my thigh bones. From this satisfaction, I drew a sense of calm; I was losing weight, therefore things would be all right. The notion sounds ridiculous now but, at the time, I associated thinness with all the things I valued: friendship, love and even success. These things could only take place in someone inhabiting a thin body. I would, naturally have to complete the prerequisite of achieving “thinness” before I could have any of those things. This belief, rather than creating a connection between the rest of my life and my experience in my body, only served to fragment my bodily experience, as I tried to form my shape into the mould I thought it should inhabit.
Fast-forward more than 10 years later. There is a sale at a store I used to frequent as a teenager. Since all my jeans have the coordinated foresight to spring holes at the same time (between the thighs, naturally), I decide to go in and try on some pants. When I realize that I take a full two sizes smaller than the last time I ever slid this brand of jeans over my hips, my chest is filled with the same contented bubbling I experienced that afternoon in photography. The anxiety of my future – my career, my empty wallet and my relationship -relaxes. I walk out with two pairs.
I am wearing the jeans on the subway when I run into my former boss. She and I chat about the weather and the school and she tells me that her young daughters refuse to wear pants because “they encumber their knees at circle time.” We chuckle at the humor of the situation and my mind travels to my closely wrapped thighs, feels the snugness of denim surrounding them. For me, pants serve as a container for the flesh that threatens to spill out of them. I remember wondering when my definition of “comfort” evolved from the freedom of the body to expand, move and breathe to this feeling of secure confinement I experience inside my jeans. I doubt these pants would allow my knees to properly stretch themselves out and bend at circle time. Luckily, when you’re pushing 30, you get to sit in chairs while people tell you stories.
As a naturopathic doctor, I preoccupy myself with the relationship our bodies have with our environment and lifestyles: how do the products we use affect our hormones? How does the food we eat and the movement we engage in affect our internal terrain? How does our mindset prevent disease? What I often don’t ask is how the learned relationship one has with their body affects health. Does the way I view my lower body cause me to engage in behaviours that affect my health? How are my tight jeans impeding lymphatic flow? How do they affect my digestion? Does my sense of self-worth affect my blood sugar? The answer is it absolutely can, if my sense of self-worth causes me to ignore my body’s food cravings and hunger signals. The way we treat ourselves and imagine our own health stems from our relationships with our bodies, which in turn dictates our future health states.
Susie Orbach, a feminist psychotherapist and author, once wrote that female babies are breastfed for less time, and picked up and cuddled less than male babies. She goes on to describe how this early treatment of women, “characterized by emotional deprivation and feelings of unentitlement”, secures the female’s place as a second-class citizen in society. More than that it teaches women to disconnect with our bodies. If our needs are not met at an early age, we are led to believe that these needs are wrong. We are taught to ignore the smelling, farting, bleeding, overflowing, curving bodies we are born with and try to recreate a “false body” that is perfect and that begins to believe it is “comfortable” being squeezed and starved and stuffed into pointy-toed shoes. Or we simply develop the ability to de-identify with the discomfort. This mechanism can lead to injury or disease if we fail to truly listen to what our bodies are trying to alert us to. (Matthew Remski writes about this extensively in his amazing research project on yoga injuries called What Are We Actually Doing in Asana (WAWADIA). I’ve been devouring his articles this week).
Orbach goes on to theorize that the symptoms the body produces in a disease state just might be a cry for help; the body is attempting to insist on its existence, to demand to be heard. So what then are menstrual cramps? Are they simply a result of inflammation or a hormonal imbalance caused by lifestyle or are they attempts made by the body to cry out, “I am female! I am menstruating! I am in need of attention!”
I remember a patient I had who would deny herself life pleasures. Convinced she needed to lose weight, she would ignore her hunger signals, even proudly telling me that she would turn to her stomach and tell it to “shut up” when the grumbling became too loud. Her chief complaint was chronic pain. I wonder if her body’s pain was simply its way of telling her it existed. I wonder if she’d have found a way to sufficiently answer her stomach’s calling, the pain would have subsided. Perhaps by listening to the experience of our bodies we can start to properly take care of our health. We can start by wearing comfortable pants that don’t “encumber the knees”, moving naturally, embracing our sexual appetites, feeding ourselves the food we truly crave and answering the need for physical touch and rest.
In a society that tends to view the body as an object, a machine that sometimes gets jammed with inconveniences such as pain, menstrual issues and eczema, I wonder how our collective health would change if we began to experience the body as a tool for healing and self-growth – something inherently wise.
To share one last story, I remember sitting across from Teresa, our school counsellor, while I was still a naturopathic student. At the time I was deciding to break up with my then-boyfriend thereby ending a 5-year relationship. I told her I had never been clear on the difference between the fear and apprehension that came with seizing something good and the repulsed feeling of avoiding something bad. This has led me to make decisions in my life that weren’t necessarily right for me. She asked me to cultivate the two feelings and locate their positions in my body. “See if there is any difference,” She told me. As I tuned in I immediately noticed that fear was closer to my heart. It was higher up and it bore the faint pleasant glow of excitement behind its initial anxiety. Disgust was located lower down. It felt like a stomach ache, a sense of doom, of indigestion: a hard-to-digest truth. It was in this moment that I fully appreciated the body’s wisdom. The old adage “listen to your gut” began to ring true to me. My gut was sending me a message that was loud and clear, but it was up to me to listen to it.
So what are some exercises we can do to cultivate body awareness and re-inhabit our bodies?
– Practice regular body scan mediations, such as those prescribed by the Mindfulness-Based Stress Reduction (MBSR) model taught by Jon Kabat-Zinn.
– Try Susie Orbach’s “Mirror Exercise” in her book Fat is a Feminist Issue or spend 3 minutes a day for 21 days staring at a body part that you have a hard time identifying with. By staring at the nose you’ve always felt was too big on a regular basis, you are able to incorporate it into your sense of self and accept it as something beautiful, in the way you would come to love the same nose on your grandfather, daughter or dear friend.
– Set a timer every hour while at work to remind yourself to tune in to your body and your breath. Notice your feet planted on the floor and move your awareness up through your feet to the top of your head. Ask yourself if there’s anything your body needs: are you thirsty, hungry, bored or lonely? Do you need to stand up and stretch? Do you need a hug?
– Get regular acupuncture or constitutional hydrotherapy to help the flow of Qi through the body.
– Finally, touch yourself. Practice ayurvedic self-massages or apply a natural moisturising lotion or oil before bed. Practice self-care in the form of hydrotherapy. Even placing the hands over the heart and breathing into that area will help to release oxytocin, a hormone responsible for love and bonding, creating feelings of calmness and attachment to the physical body.

by Dr. Talia Marcheggiani, ND | Nov 7, 2014 | Endocrinology, Fertility, Hormones, Sexual Health, Sexuality, Weight Loss, Women's health
 There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
There are many reasons to start using the birth control pill. Some of them are not-so-great: dealing with painful menstruation, acne, irregular periods or ovarian cysts – there are other, natural ways to manage these health concerns with fewer side effects and health risks! Some reasons for going back on the pill after a few-year hiatus are pretty awesome, like starting a new relationship. In other words, using the birth control pill for what it was designed for: birth control.
I’m surprised to find that I’m hesitant to admit it publicly, but I’ve decided to go back on The Pill after considering various contraception methods; in natural health circles the Birth Control Pill is often seen as an unnecessary evil. However, Tori Hudson author of the Women’s Encyclopedia of Natural Medicine, has called oral contraceptives a “truly revolutionary option for women” and points out that the dose of estrogen and progesterone in the pill today is much lower than it was when it first arrived on the market. That being said, it’s important to talk to a healthcare provider to go over birth control methods and decide which one is right for you. Alternate options include physical barriers, such as condoms and diaphragms, cycle charting, apps, such as the Lady Comp, or IUDs, to name a few. Each method has its associated pros, cons, costs and health risks. Finding a safe and effective form of contraception involves you and your healthcare team.
For me, The Pill seems to be the best choice at the moment for various reasons, which I won’t get into here. However, the idea of ingesting synthetic hormones again, after having carefully brought my cycles back to a perfect, painless and PMS-free 28-day rotation and after having cleared up my hormonal acne, made me nervous. So, I did what all trained naturopathic doctors do; I used my naturopathic know-how to tailor an optimal Synthetic Hormonal Experience for myself. Going back on the pill needn’t come with undesirable side effects; maybe it could be a positive experience. Here are some tips:
Decide if oral contraception is your best method
Selecting the method of birth control that best fits your lifestyle, budget, health history and personal style requires an in-depth conversation between you and your healthcare provider. He or she should have a detailed conversation with you about your expectations, goals, sexual and health history as well as family history. Selecting the right method may also require some trial and error.
Consider the associated risks
A history of smoking and blood clots could put you at risk for dangerous side effects. The birth control pill is also associated with an increased risk of certain cancers. (And a decreased risk of uterine and ovarian cancers in the general, healthy population). Your personal risk profile will involve your personal health history and family history as well as lifestyle factors such as smoking. Talk to your healthcare provider.
Pick the right pill for you
Based on my history of suboptimal glucose control, hormonal acne and irregular periods, I knew that I needed a pill with the lowest dose of estrogen possible. My hormonal profile tends towards estrogen dominant and progesterone deficient so I chose a low-dose estrogen and high-dose progestin pill. The form of progestin used has zero androgen (male hormone) activity, therefore it is unlikely to contribute to acne. It also contains a diuretic, which combats my tendency to hormone-related water-retention. The combination of my knowledge of my personal hormonal profile and ability to research hormone combinations in various pills led me to choose a product that offered positive side-effects rather than negative ones. Since being on the pill again, I’ve experienced weight loss, rather than gain, lighter, more regular cycles and clearer skin. It’s worth repeating that these side-effects were not my motivation for going on the pill. If you are using the pill for symptom-management and hormone-balancing rather than birth control, consider trying natural methods instead.
Be prepared for trial and error-ing as hormone levels fluctuate
Give your new pill a 3-month trial period. During this period, be prepared for temporary side effects such as mood changes, skin outbreaks, temporary weight gain or water retention and break-through bleeding. Other common side effects of synthetic hormones are nausea and headaches. Allow 3 months for things to stabilize and, if still experiencing symptoms, talk to your healthcare provider about trying a new pill or birth control method.
Make sure to supplement to account for vitamin and mineral deficiencies
Oral contraceptives can deplete several key vitamins and minerals. The B vitamins folate, B6 and vitamin B12 are most notably affected. Deficiencies in these vitamins could lead to fatigue and depression or even neurological impairment. Magnesium, zinc and vitamin C levels are also affected, which can have an impact on the immune system. These minerals are important in a variety of metabolic processes. Since starting the pill again, I am diligent about taking my B-complex and magnesium supplements. Make sure you talk to your naturopathic doctor or other healthcare provider about choosing a quality supplement and dosing correctly, to make sure you are putting back in your body the nutrients that your pill may be depleting.
Hormone balance when coming off the pill
If you reach a happy medium with your pill, then congratulations! But, you ask, what happens if I decide to get pregnant or switch to another method of birth control? Work with a naturopathic doctor or your trusted healthcare provider to balance hormones with herbal or nutritional supplements when coming off of the pill. Herbs such as vitex, help regulate hormones and prevent side effects from the withdrawal of synthetic hormones.
For more information on balancing hormones and optimizing fertility, contact me.
This article is not a substitute for medical advice.

by Dr. Talia Marcheggiani, ND | May 31, 2013 | Exercise, Health, Outdoors, Paleo, Parks, Pets, Weight Loss

Despite having had a brief love affair with virtually every form of cardio exercise, I still remain attached to my one true love: walking. Once not even considered exercise in many gym circles, we now know it’s one of the best forms of movement out there. Here’s some reasons why it’s so good for you and some tips on how to do it right:
(more…)

by Dr. Talia Marcheggiani, ND | Mar 21, 2013 | Balance, Emotions, Fitness, Health, Mental Health, Mindfulness, Motivation, Nature Cure, Naturopathic Philosophy, Naturopathic Principles, Self-care, Treating the Cause, Weight Loss, Women's health

This article was first published in My Yoga Online.
With the growing rates of obesity in our society, combined with the tendency for most people who successfully lose weight to gain it back only a short while later, it’s obvious that something is flawed in our society’s general weight-loss strategy.
(more…)

by Dr. Talia Marcheggiani, ND | Jan 11, 2013 | Body Image, Nutrition, Research, Weight Loss

The new year brings with it the onslaught of new year’s resolutions, the most common being, of course, to lose weight. While most people think that losing weight can help them better their health and well-being, a new study published in JAMA begs to differ.
(more…)